Unusual Metastasis from Follicular Thyroid Carcinoma: A Case Report and Literature Review
Abstract
Introduction
Follicular thyroid carcinoma (FTC) is a type of well-differentiated thyroid carcinoma. It has a poorer prognosis, is more metastatic, and has characteristics different from papillary thyroid carcinoma. It tends to metastasize hematogenously, usually to the bones and lungs. This study aims to present a rare case of FTC metastasis to the peritoneum and thigh of a patient with a literature review.
Case presentation
A 70-year-old patient presented with a right thigh mass. Magnetic resonance imaging of the right thigh revealed an intramedullary lesion in the femoral diaphysis. The thyroid gland was firm, with no evidence of enlargement. A computed tomography scan showed several peritoneal nodules. A core biopsy of the right upper femoral lesion and peritoneal mass was performed. Histopathologic findings and immunohistochemical analysis confirmed metastatic FTC with thyroid origin.
Literature review
Unlike widely invasive FTC, minimally invasive FTC has a better prognosis and is less metastatic. Imaging, histopathologic examination, and immunohistochemistry can help in arriving at a diagnosis of FTC. Mutations of PPAR-γ and RAS are associated with FTC. Radioiodine treatment and suppressive therapy for the thyroid-stimulating hormone have been shown to improve survival rates of FTC, with postoperative follow-ups and treatment being important.
Conclusion
Metastasis of FTC to the peritoneum is rare and could lead to a late diagnosis. Proper diagnosis with confirmatory tools such as immunohistochemistry and adequate treatment are critical.
Introduction
Follicular thyroid carcinoma (FTC) is an infrequent type of thyroid carcinoma that represents approximately 10% of all thyroid cancers [1]. Together with papillary thyroid carcinoma (PTC), they are classified as well-differentiated thyroid malignancies, which make up over 85% of all thyroid carcinoma cases. FTC, however, has genetic mutations, pathological characteristics, and a poorer prognosis different from PTC [2]. Follicular adenomas occur more frequently than follicular carcinomas. Follicular carcinomas are distinguished from follicular adenomas by microscopic evidence of vascular or capsular invasion [3]. Follicular thyroid cancer tends to spread through the bloodstream, which may account for its higher rate of distant metastasis compared to PTC [4]. Spreading via the lymphatic system can also occur but is rarer [3]. Distant metastasis occurs in around 6-20% of cases of FTC, with the bones and lungs being the most affected sites [4]. The tumor tends to present at a relatively older age and is associated with a higher rate of mortality compared to PTC [5]. The mortality rate of FTC is around 10–30% [6]. Metastasis is considered the most critical factor influencing survival outcomes in FTC. Sometimes, distant metastases could be the first sign of the disease, as some cases are only found after the cancer has spread to other body parts, while in others, they can appear following initial treatment [2]. Metastasis of FTC to the peritoneum is exceedingly rare. This study aims to showcase a very rare case of FTC metastasis to the peritoneum, along with the patient's thigh, combined with a literature review. The cited references in this case report have been assessed for reliability [7] and compiled with CaReL guidelines [8].
Case presentation
Patient information
A 70-year-old female patient presented with a right thigh mass that had been present for two weeks. She is a non-smoker with a known history of diabetes mellitus, currently managed with anti-diabetic medication. The patient underwent thyroid surgery in 2011. However, the histopathology report from the procedure was unavailable. She is presently taking levothyroxine 100 mcg once daily.
Clinical findings
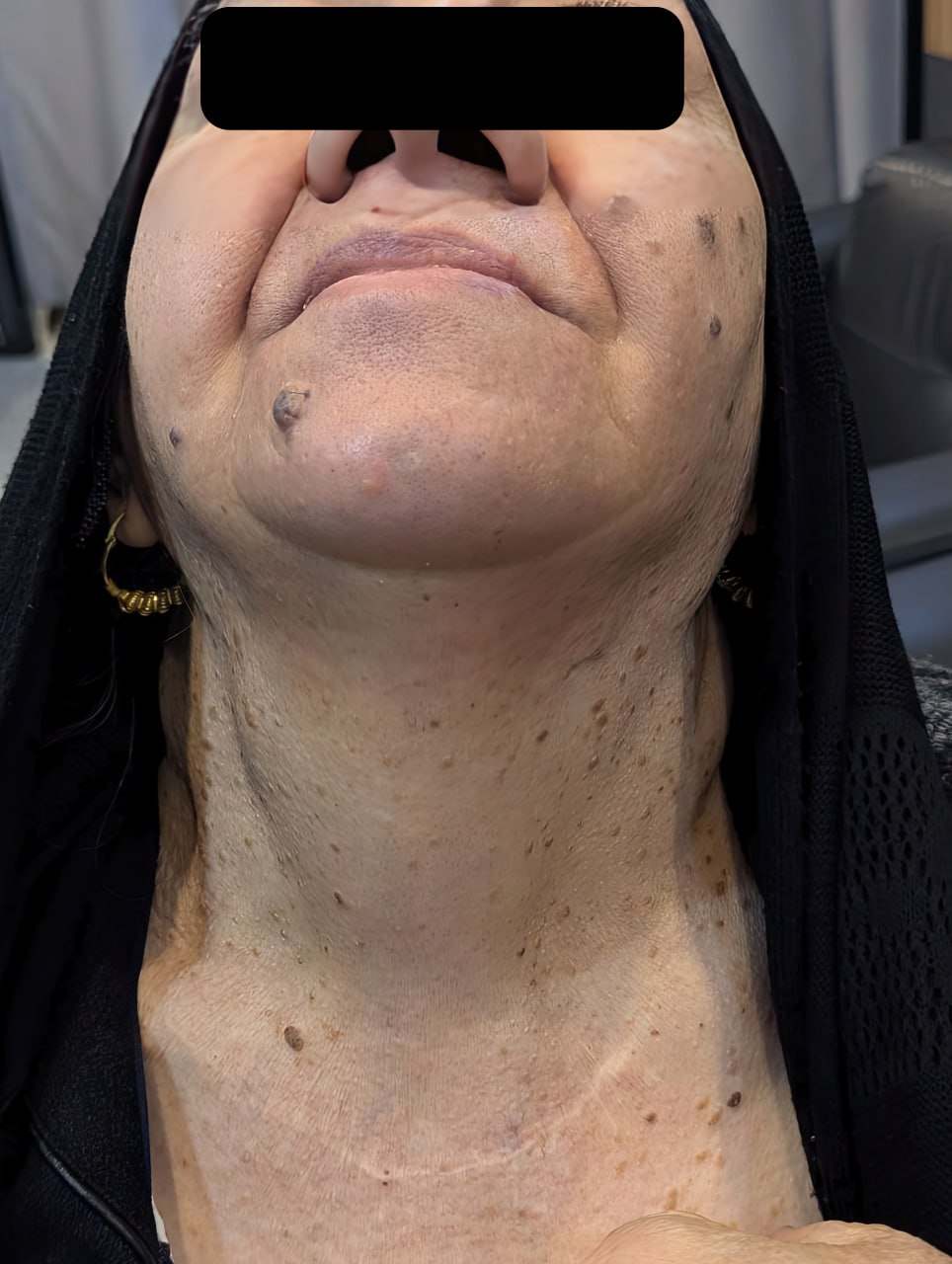
The patient was vitally stable. On examination of the neck, the thyroid gland was found to be firm bilaterally upon examination, with no evidence of enlargement (Figure 1). No palpable cervical lymphadenopathy was detected. A small lymph node identified during evaluation demonstrated only reactive changes on histological examination.
Diagnostic approach
Magnetic resonance imaging of the right thigh revealed a 35 × 48 mm intramedullary lesion in the femoral diaphysis. The lesion demonstrated low signal intensity on T1 and intermediate signal intensity on T2 with homogeneous post-contrast enhancement. It was associated with cortical destruction and extraosseous soft tissue extension. These imaging features are suggestive of metastatic involvement, warranting histopathological confirmation. A computed tomography scan of the chest and abdomen revealed multiple lung nodules, with the largest measuring 27 mm. Additionally, several peritoneal nodules were identified in the right and mid-anterior abdominal regions, the largest measuring 18 mm. These findings were suggestive of metastatic disease.
A core biopsy of the right upper femoral lesion was performed, confirming metastatic carcinoma. Immunohistochemical analysis suggested a thyroid origin. Laboratory investigations included thyroid function tests, which revealed that thyroid-stimulating hormone (TSH) level was 0.548 µIU/mL (normal range: 0.8–6.0 µIU/mL), free T4 was 21.5 pmol/L (normal range: 12.8–27 pmol/L), calcitonin (CATN) was <0.5 pg/mL (normal range: up to 9.82 pg/mL), thyroglobulin (Tg) was >500 ng/mL (normal range: 3.5–77 ng/mL), serum calcium was 9.83 mg/dL (normal range: 8.8–10.8 mg/dL), and parathyroid hormone (PTH) was 33.3 pg/mL (normal range: 15–65 pg/mL).
A neck ultrasound showed a remnant right lobe measuring 33 × 14 × 7 mm with a solid, heterogeneous echotexture. A smaller nodule measuring 12 × 7 × 4 mm of remnant tissue was detected below the lower pole of the previously noted remnant. In the midline of the neck, over the thyroid cartilage, an isoechoic, hypovascular remnant tissue measuring 15 × 6 × 4 mm was observed. The remnant left lobe measured 34 × 12 × 12 mm with a solid, heterogeneous echotexture containing a small TI-RADS 4 nodule measuring 6 × 6 × 4 mm. The isthmus was absent.
Additionally, a few small, solid, hypoechoic, hypovascular nodules were observed in the operative bed, with the largest measuring 5 × 3 mm in the left thyroid bed. Small lymph node-like structures were also noted. The patient underwent a core biopsy of the peritoneal mass. Histopathologic examination showed cores of fibrofatty tissue infiltrated by sheets of variably sized follicles that were lined by cuboidal cells with a moderate amount of eosinophilic to clear cytoplasm and round, hyperchromatic nuclei, some of which had conspicuous nucleoli. Eosinophilic colloid material was present in the lumina of some of the follicles. There was no notable mitotic activity or necrosis. There was a mild lymphoplasmacytic infiltrate in the fibrous tissue (Figure 2). Immunohistochemistry showed positive staining of the tumour cells for CK7 (cytoplasmic staining of moderate intensity in 70% of the tumour cells), PAX-8 (nuclear staining of moderate intensity in 100% of the tumour cells), and TTF-1 (nuclear staining of strong intensity in 100% of the tumour cells). These findings confirmed the diagnosis of metastatic follicular thyroid carcinoma to the peritoneum (Figure 3).
Therapeutic intervention
Following a comprehensive evaluation by a multidisciplinary team, the patient was scheduled for radioactive iodine ablation and subsequently underwent a total revision thyroidectomy. Both recurrent laryngeal nerves were successfully preserved. The excised tissue was submitted for histopathological examination, which revealed nodular Hashimoto’s thyroiditis with adenomatoid nodules and multiple reactive lymph nodes but no malignancy. The patient’s vital signs remained stable with smooth postoperative recovery. The peritoneal metastasis was managed with a plan for radioactive iodine ablation. Considering the patient’s clinical stability and the iodine-avid characteristics of the lesions, she was deemed an appropriate candidate for the therapy and was subsequently scheduled to receive it.
Follow-up and outcome
The patient recovered well postoperatively without complications. She was subsequently referred for radioactive iodine ablation and to an oncologist for ongoing follow-up and management. Her condition remains clinically stable, and she continues to be monitored pending treatment.
Discussion
Well-differentiated thyroid cancers like FTC and PTC will rarely metastasize to locations other than bones, lungs, and lymph nodes. Nonetheless, the occurrence of this small probability can lead to a late diagnosis [9]. Distant metastases to sites such as the brain, liver, breasts, muscles, kidneys, and skin are uncommon or occur infrequently. Distant metastasis is the most critical negative prognostic indicator; around 50% of affected patients survive beyond 10 years [10]. There is scant documentation of FTC metastasis to the peritoneum or abdominal area, with only a few case reports [11]. A struma ovarii containing FTC and metastasizing or spreading to the peritoneum can also occur [12, 13]. Mesentery metastasis of said carcinoma is rare as well [14]. Some cases of differentiated thyroid carcinoma metastases or spread to the peritoneum in literature have been reviewed in (Table 1) [11-15]. Iodine-sufficient and iodine-deficient regions show different ratios of papillary to follicular thyroid carcinoma, with iodine-deficient areas typically having lower ratios. Consequently, dietary iodine supplementation causes an increase in the said ratio [16].
|
Author and year of publication |
Age |
Sex |
Diagnosis |
Clinical findings |
Imaging |
Immunohistochemical tests |
Treatment |
Postoperative care |
Outcome |
|
Hamdy et al. 2024 [12] |
22 |
F |
left ovarian highly differentiated FTC from struma ovarii with peritoneal and omental spread. |
Iliac fossa pain, hypomenorrhea, & palpable lower abdominal mass. |
US: multicystic pelviabdominal lesion. Post-contrast MRI: midline multi-locular pelviabdominal left ovarian cystic mass. |
IHC: +ve TTF1, & Tg. |
Left salpingo-oophorectomy, omental & peritoneal biopsies, & thyroidectomy. |
Radioactive iodine treatment, & levothyroxine. |
Is in stable condition. |
|
Porntharukchareon et al. 2023 [11] |
44 |
F |
FTC metastasis to peritoneum. |
Multiple peritoneal nodules, low FT4 & normal TSH levels. |
CT of the peritoneum negative. US: small left thyroid nodule. |
IHC: +ve CK-7, Tg, & TTF-1. |
Total thyroidectomy. |
Radioactive iodine treatment. |
Is in stable condition. |
|
Chwa et al. 2023 [14] |
62 |
M |
Metastatic FTC on mesentery. |
Mesentery mass during check-up. |
PET/CT: mesentery mass. Chest CT: enhancing nodule in the left lower lobe. |
IHC: < 3% Ki-67. |
Lung lower lobe wedge resection, mesentery mass, & small bowel segment removed. |
Radioactive iodine treatment. |
Is in stable condition. |
|
Miles et al. 2016 [15] |
68 |
F |
Primary pelvic PTC metastasis to peritoneal surface. |
Urinary retention. |
US: heterogeneous pelvic mass. MRI: deep central pelvic mass like a uterus solid leiomyoma with extensive central necrosis. |
IHC supported the diagnosis of thyroid carcinoma. |
Surgically resected retroperitoneal mass, total hysterectomy, resected superficial peritoneum tumor implants, & elective total thyroidectomy after 3 months. |
Radioactive iodine treatment. |
Is in stable condition. |
|
Choi et al. 2012 [13] |
33 |
F |
Peritoneal dissemination of follicular carcinoma arising from struma ovarii. |
Enlarged uterus. |
MRI: bilateral par-ovarian solid tumors & unusual metastatic lesions manifestation in the pelvic cavity. |
Peritoneal mass HPE: thyroid gland enveloped in a fibrous capsule. |
Exploratory laparotomy under the impression of bilateral ovarian malignancy, total thyroidectomy. |
Radioactive iodine treatment. |
Is in stable condition. |
When it comes to FTC, it can be cytologically very similar to follicular thyroid adenoma, unlike papillary carcinoma, which is typically easy to diagnose due to its distinctive nuclear features and growth pattern. In such situations, the growth pattern of the tumor (particularly the presence of capsular and/or vascular invasion) can be used to differentiate carcinoma from adenoma [17]. Follicular thyroid adenomas and FTC also have distinct microarray expression profiles, which set them apart from each other, with FTC showing more overexpression of autotaxin, EMMPRIN, GADD153, and galectin-3 mRNAs, and follicular thyroid adenomas showing increased TFF3 mRNA expression [18]. Follicular thyroid cancer can be classified into minimally invasive FTC, widely invasive FTC, and encapsulated angioinvasive FTC, with minimally invasive FTC having a better prognosis and being less metastatic. In contrast, widely invasive FTC is typically associated with a larger tumor, occurring in older individuals, more invasive growth into the thyroid, and distant metastasis [2]. Both minimally invasive FTC and widely invasive FTC show a lack of cytological atypia. Histological features required for FTC diagnosis include angioinvasion and/or invasion that penetrates the full thickness of the tumor-surrounding capsule [17]. Multiple factors affect FTC prognosis, including the presence of residual tumor after surgery, the patient's age, whether there is local or distant metastasis, the size of the tumor, and the tumor's pathological classification [1]. On ultrasonography, the presence of microcalcifications, which may indicate the presence of psammoma bodies, is rare in FTC and common in PTC. At the same time, both PTC and FTC could have rim and coarse calcifications [16].
Immunohistochemistry can be handy in confirming the thyroid origin of a metastatic tumor [19]. In this case, each of CK7, PAX-8, and TTF-1 were utilized to diagnose and confirm metastatic origin. TTF-1 and PAX-8 can be produced in the lung and kidney, respectively. However, they are co-expressed with one another in thyroid follicular cells, highlighting the importance of this specific combination for establishing the thyroid of the tumor [20]. CK7 is a type of cytokeratin with a low molecular weight, an intermediate filament protein specific to epithelial cells, and it is typically found in glandular epithelium. It is more commonly used in diagnosing tumors outside the thyroid, where it helps determine the tumor’s origin, rather than in tumors within the thyroid gland itself. It may also be used with CK20 to help with the diagnosis, with CK7 positivity accompanied by CK20 negativity being found in a few organs including the thyroid [19]. The thyroid-specific enhancer-binding protein TTF-1 can also help confirm a tumor’s thyroid origin, but not in differentiating among different thyroid lesions, with positive results found in around three-quarters of thyroid carcinoma metastases [19]. Li et al. utilized TTF-1 and CK7 positivity, along with thyroglobulin and partial CD56 positivity, in their immunohistochemical analyses to help confirm metastatic FTC in a chest wall lymph node [21].
Thyroglobulin is close to TTF-1 when it comes to sensitivity in identifying primary and secondary thyroid follicular lesions, but with these antibodies together, their diagnostic sensitivity may increase [19]. Serum thyroglobulin can be a dependable marker for detecting metastasis or recurrence since it has a 30-hour half-life following a total thyroidectomy [14]. Olejarski et al. report a 73-year-old with a right thigh soft tissue mass, surrounding a right proximal-mid femoral prosthesis on a computed tomography scan. A core biopsy of the mass revealed a follicular lesion showing positive results for TTF-1 and thyroglobulin, indicating a metastatic tumor of thyroid origin. The patient showed an elevated serum thyroglobulin indicative of a significant volume disease [22]. Genetic mutations associated with FTC include mutations of PPAR-γ and the mitogen-activated protein kinase activator and PI3K-AKT pathways known as RAS, which is frequently found in follicular adenomas, indicating a role in its early tumorigenesis. Other mutations are required to transform the adenoma into a carcinoma, such as PIK3CA mutations and PTEN, a tumor suppressor gene [16].
When the cytological or ultrasound findings indicate a higher risk of cancer, or if malignancy is present and to allow for radioiodine treatment postoperatively, total thyroidectomy may be considered [23]. Grani et al. found several studies showcasing that patients with FTC who were given radioiodine treatment had better chances of survival than those patients who did not. Another one showed that patients with distant metastases had improved chances of survival with radioiodine treatment, and in those without distant metastases, it increased local control. They also found several studies that showed better results with suppressive therapy for the thyroid-stimulating hormone after the initial treatment. External beam radiotherapy is also linked to better relapse-free survival for FTC when treating local or distant areas [16]. Post-therapy 131I whole-body scintigraphy and 131I single photon emission computed tomography/computed tomography are essential for patient management in differentiated thyroid carcinomas due to their high sensitivity and specificity [10]. Miles et al., for example, made use of whole-body radioactive iodine scanning for their patient with primary pelvic PTC metastasis to the peritoneal surface after the surgeries to follow up on the patient’s condition. In it, two faint areas of activity were seen on the right side of the thyroid region, likely indicating small remnants of thyroid tissue, along with a small but clearly defined area of activity in the pelvic region, helping in the patient’s management as they got better [15].
Conclusion
The rarity of FTC metastasis to locations like the peritoneum could lead to a late diagnosis and complications. Thus, it is critical to consider this probability, make proper diagnoses with tools such as immunohistochemistry, and treat accordingly.
Declarations
Conflicts of interest: The authors have no conflicts of interest to disclose.
Ethical approval: Not applicable.
Patient consent (participation and publication): Written informed consent was obtained from the patient for publication.
Funding: The present study received no financial support.
Acknowledgements: None to be declared.
Authors' contributions: AMS and DAI were significant contributors to the conception of the study and the literature search for related studies. AHA was the radiologist who performed the assessment of the case. RMS was the pathologist who performed the histopathological diagnosis. TOS and HAA were involved in the literature review, study design, and manuscript writing. KMS, AMA, and SHH were involved in the literature review, the study's design, and the critical revision of the manuscript, and they participated in data collection. SSA and MMA confirm the authenticity of all the raw data. All authors approved the final version of the manuscript.
Use of AI: ChatGPT version 5.2 (OpenAI) was used solely for language editing, paraphrasing, and improvement of clarity and grammar in this manuscript. The artificial intelligence tool did not contribute to the study design, data collection, data analysis, data interpretation, or the generation of scientific content. All outputs produced with the assistance of ChatGPT were carefully reviewed, verified, and approved by the authors. The authors take full responsibility for the accuracy, integrity, and originality of the entire manuscript.
Data availability statement: The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
- Salih AM, Abdullah AM, Baba HO, Omer GL, Habibullah IJ, Muhialdeen AS, et al. Insular thyroid carcinoma in the background of follicular thyroid carcinoma: A report of a rare case and mini review of the literature. World Academy of Sciences Journal. 2024;6(4):32. doi:10.3892/wasj.2024.247
- Wu MH, Lee YY, Lu YL, Lin SF. Risk factors and prognosis for metastatic follicular thyroid cancer. Frontiers in endocrinology. 2022; 13:791826. doi:10.3389/fendo.2022.791826
- Cai DM, Wang HY, Jiang Y, Parajuly SS, Tian YE, Ma BY, et al. Primary follicular thyroid carcinoma metastasis to the kidney and widespread dissemination: A case report. Oncology Letters. 2016;11(5):3293-7. doi:10.3892/ol.2016.4417
- Omar B, Yassir H, Youssef O, Sami R, Larbi AR, Mohamed R, et al. A rare case of follicular thyroid carcinoma metastasis to the sacral region: A case report with literature review. International Journal of Surgery Case Reports. 2022; 94:107001. doi:10.1016/j.ijscr.2022.107001
- Liu Y, Liu X, Chen X, Zhou L, Gao X, Yu H. Follicular thyroid carcinoma presenting with multiple skull metastases on CT and MRI: a case report and literature review. Radiology Case Reports. 2021 Nov 1;16(11):3260-5. doi:10.1016/j.radcr.2021.07.054
- Zhang T, He L, Wang Z, Dong W, Sun W, Zhang P, et al. Risk factors for death of follicular thyroid carcinoma: a systematic review and meta-analysis. Endocrine. 2023;82(3):457-66. doi:10.1007/s12020-023-03466-9
- Abdullah HO, Abdalla BA, Kakamad FH, Ahmed JO, Baba HO, Hassan MN, et al. Predatory Publishing Lists: A Review on the Ongoing Battle Against Fraudulent Actions. Barw Medical Journal. 2024;2(3):26-30 doi:10.58742/bmj.v2i2.91
- Prasad S, Nassar M, Azzam AY, García-Muro-San José F, Jamee M, Sliman RK, et al. CaReL guidelines: A consensus-based guideline on case reports and literature review (CaReL). Barw Medical Journal. 2024. doi:10.58742/bmj.v2i2.89
- Madani A, Jozaghi Y, Tabah R, How J, Mitmaker E. Rare metastases of well-differentiated thyroid cancers: a systematic review. Annals of Surgical Oncology. 2015; 22:460-6. doi:10.1245/s10434-014-4058-y
- Song HJ, Xue YL, Xu YH, Qiu ZL, Luo QY. Rare metastases of differentiated thyroid carcinoma: pictorial review. Endocrine-related cancer. 2011;18(5):R165-74. doi:10.1530/ERC-11-0068
- Porntharukchareon T, Mahasandanaa T, Samdaengpan C, Sricharunrat T, Kunawudhi A. a rare case of peritoneal metastasis from follicular thyroid carcinoma without primary lesion in a patient with hypopituitarism. Journal of the ASEAN Federation of Endocrine Societies. 2023;38(S3):103-. doi:10.15605/jafes.038.AFES.176
- Hamdy O, Nassar AN, Hassan A, Hassan A, Eldesoky RT, Saleh G. Highly differentiated follicular carcinoma of the ovary with omental and peritoneal spread in a 22-year-old girl; A diagnostic and counseling challenge. International Journal of Surgery Case Reports. 2024 Apr 1; 117:109464. doi:10.1016/j.ijscr.2024.109464
- Choi BR, Kim BW, Yoon SO, Kim YT, Lee S, Kim JH. Peritoneal dissemination of follicular carcinoma arising from struma ovarii in a pregnant woman. Korean Journal of Obstetrics & Gynecology. 2012;55(12):1006-9. doi:10.5468/KJOG.2012.55.12.1006
- Chwa S, Lee SH, Lee SH. Unusual mesentery metastasis of differentiated thyroid cancer: a case report. Korean Journal of Clinical Oncology. 2023;19(2):84. doi:10.14216/kjco.23015
- Miles M, Ward C, Pezzi CM, Kelley CA, Pezzi T, Seelaus J, et al. Primary Pelvic Papillary Thyroid Carcinoma with Metastases to Peritoneal Surfaces. The American Surgeon. 2016;82(11):1148-50. doi:10.1177/000313481608201136
- Grani G, Lamartina L, Durante C, Filetti S, Cooper DS. Follicular thyroid cancer and Hürthle cell carcinoma: challenges in diagnosis, treatment, and clinical management. The Lancet Diabetes & Endocrinology. 2018;6(6):500-14. doi:10.1016/S2213-8587(17)30325-X
- Hinsch N, Frank M, Döring C, Vorländer C, Hansmann ML. QPRT: a potential marker for follicular thyroid carcinoma including minimal invasive variant; a gene expression, RNA and immunohistochemical study. BMC cancer. 2009; 9:1-8. doi:10.1186/1471-2407-9-93
- Bryson PC, Shores CG, Hart C, Thorne L, Patel MR, Richey L, et al. Zanation AM. Immunohistochemical distinction of follicular thyroid adenomas and follicular carcinomas. Archives of Otolaryngology–Head & Neck Surgery. 2008;134(6):581-6. doi:10.1001/archotol.134.6.581
- Rezk S, Khan A. Role of immunohistochemistry in the diagnosis and progression of follicular epithelium-derived thyroid carcinoma. Applied Immunohistochemistry & Molecular Morphology. 2005;13(3):256-64. doi:10.1097/01.pai.0000142823.56602.fe
- Fabbro D, Di Loreto C, Beltrami CA, Belfiore A, Di Lauro R, Damante G. Expression of thyroid-specific transcription factors TTF-1 and PAX-8 in human thyroid neoplasms. Cancer research. 1994;54(17):4744-9. doi:N/A
- Li T, Ma Z, Lu C, Zhou Q, Feng Z, Wu X, et al. Chest wall lymph node metastasis from follicular thyroid carcinoma: a rare case report. Diagnostic pathology. 2019; 14:1-6. doi:10.1186/s13000-019-0907-0
- Olejarski J, Yang M, Varghese J. Follicular thyroid carcinoma presenting as a soft tissue thigh mass. The Lancet Diabetes & Endocrinology. 2014;2(4):348. doi:10.1016/S2213-8587(14)70058-0
- Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26(1):1-33. doi:10.1089/thy.2015.0020

This work is licensed under a Creative Commons Attribution 4.0 International License.

