Exploring the Efficacy of Once and Twice Weekly Thyroxine Dosing: A Promising Approach for Hypothyroidism Management
Abstract
Introduction
Hypothyroidism is a common endocrine disorder, in which the management involves daily intake of thyroxine. However, adherence to a daily medication regimen poses a substantial challenge for many patients. The current study aims to assess the efficacy of once and twice-weekly thyroxine regimen for the management of hypothyroidism.
Methods
This was a single-center cohort study involving hypothyroid patients that was conducted over three years. In this study, standard daily, once and twice-weekly thyroxine dosing regimens were used to treat the patients. The effectiveness of the three dosage regimens was ascertained by whether the patients achieved a euthyroid state after six months of therapy.
Results
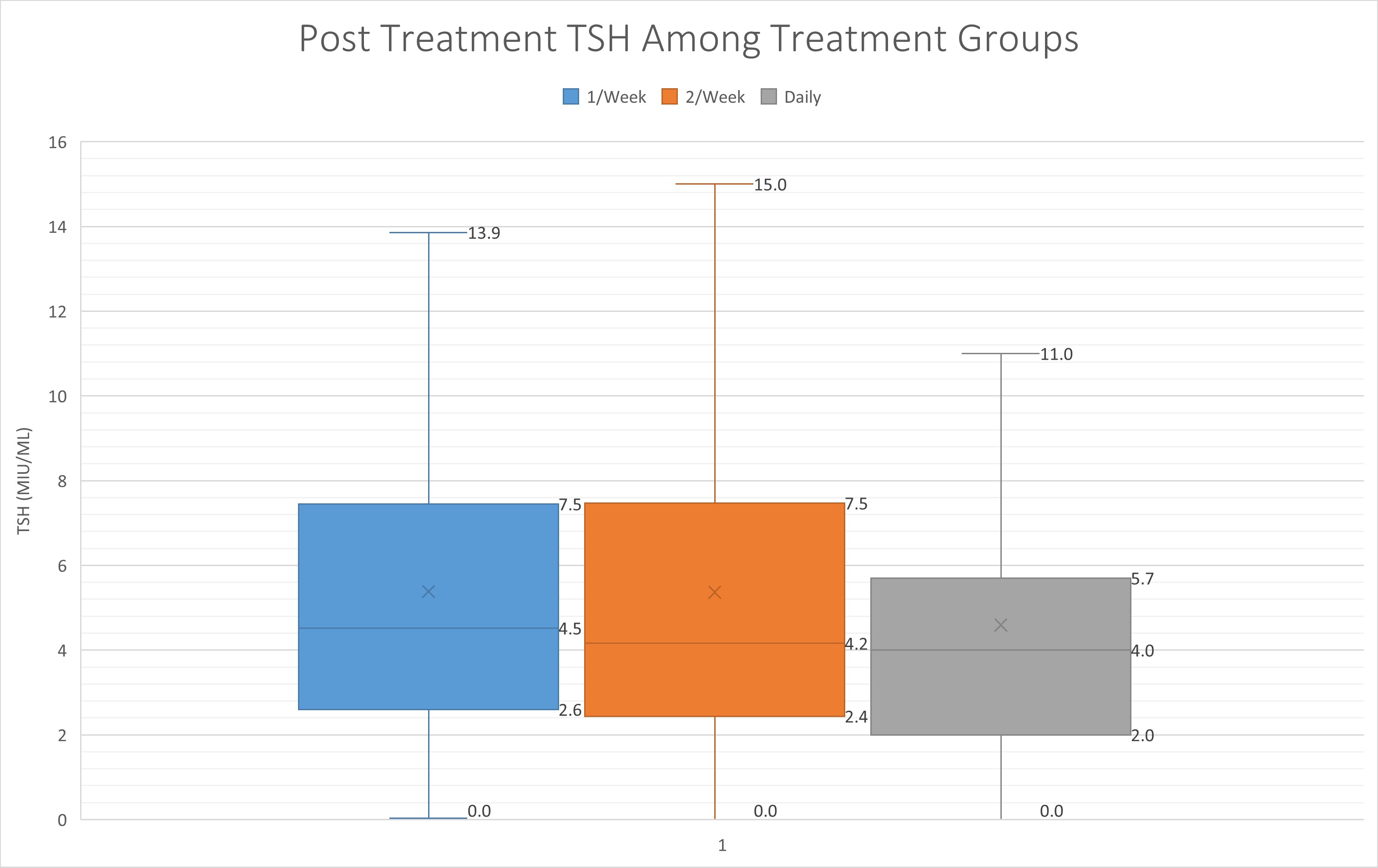
In total, 328 hypothyroid cases due to thyroiditis were included in this study. The average age of the cases was 42.7 years (14-92). Before thyroxine therapy, in the standard daily regimen group, the median level of TSH was 15.4 μIU/mL (IQR 23.1), in the once-weekly regimen group, the level was 9.2 μIU/mL (IQR 6.8), and in the twice-weekly regimen group, the level was 9.1 μIU/mL (IQR 7.3). After thyroxine intake and upon follow-up after 6 months, the TSH level decreased to 4.0 μIU/mL (IQR 3.7), 4.5 μIU/mL (IQR 4.9) and 4.2 μIU/mL (IQR 5.1) in the standard daily, once- and twice-weekly regimen groups, respectively.
Conclusion
Once and twice weekly thyroxine shows promise as strategies for managing hypothyroidism. However, variability in patients in response to weekly thyroxine needs to be taken into account.
Introduction
Hypothyroidism is a condition characterized by the inadequate production of thyroid hormones and represents a common endocrine disorder affecting a significant proportion of the global population [1]. The standard management of this condition typically involves daily administration of synthetic thyroxine to normalize thyroid hormone levels, thereby alleviating associated symptoms and metabolic disturbances. Daily thyroxine therapy regimen is well-established in clinical practice, with its efficacy extensively documented in the medical literature [1,2]. However, adherence to a daily medication regimen can be challenging for many patients. Factors such as the requirement to take the medication on an empty stomach, the necessary waiting period before the next meals or beverages, and potential drug interactions may contribute to inconsistent compliance. Suboptimal adherence to daily thyroxine therapy can significantly impair the management of hypothyroidism, resulting in inadequate control of thyroid function and poorer patient outcomes [3].
Recently, non-daily alternative dosing schedules, specifically once or twice-weekly thyroxine administration, have gained attention as potential strategies to improve adherence. Nevertheless, studies evaluating the efficacy of these regimens remain limited, and current evidence is insufficient to support changes in clinical practice. The current study aims to assess the efficacy of once and twice-weekly thyroxine dosing compared to standard daily administration for the management of hypothyroidism.
Methods
Study design
This was a single-center cohort study conducted at the head and neck center of Smart Health Tower, Sulaimani, Iraq, from January 2020 to January 2023. It involved the retrospective analysis of a series of hypothyroid cases to evaluate the efficacy of once and twice-weekly thyroxine regimens compared to standard daily dose. Written informed consent was obtained from the patients and the family of the patients.
Participation
Participants were individuals who visited the head and neck center for the treatment of hypothyroidism. Patients who had undergone thyroidectomy were excluded from the study to avoid confounding effects on thyroid function.
Treatment plan
Patients were assigned to one of three treatment groups based on the prescribed thyroxine regimen: daily, once-weekly, or twice-weekly. According to thyroid function tests and body weight, different daily and weekly doses were prescribed to the patients to reach euthyroidism, including 25, 50, 75, or 100 μg per day, or 100, 200, or 300 μg per week. Patients were followed for six months, and treatment effectiveness was determined by whether they achieved a euthyroid state, defined as a thyroid stimulating hormone (TSH) level between 0.4 and 4.2 μIU/mL.
Data collection and analysis
Data were extracted from the center’s medical database and included patient’s age, gender, marital status, occupation, chief complaint, thyroxine dosage, TSH pre-treatment, and TSH six months following therapy. All data were entered into an Excel spreadsheet (2016). Statistical analyses were performed using statistical package for social sciences (SPSS) version 25. Descriptive statistics were presented as means or medians (for non-normally distributed data), counts, and percentages. Univariate analyses were conducted to compare baseline characteristics (including age, gender, marital status, occupation, and chief complaint) and treatment outcomes between groups. Additionally, multivariate logistic regression analysis was performed to identify independent predictors of achieving normal TSH (0.4–4.2 μIU/mL) at six months. A p-value of less than 0.05 was considered statistically significant.
Results
In total, 328 hypothyroid cases due to thyroiditis were included in this study. The mean age of the cases was 42.7 years, ranging from 14 to 92 years. The majority of the cases were female, accounting for 303 individuals (92.4%). The most common presentation in all groups was weakness in 146 (44.5%) cases, followed by incidental finding in 81 (24.7%), and neck pain in 37 (11.3%). Overall, the first TSH mean (before therapy) was 20.8, while the second TSH mean (after treatment) was 5.1 (Table 1).
|
Characteristics |
Frequency/Mean |
Percentage/SD |
|
Age |
42.7 |
13.1 |
|
First TSH |
20.8 |
25.1 |
|
Second TSH |
5.1 |
4.2 |
|
Sex |
||
|
Male Female |
25 303 |
7.6 92.4 |
|
Occupation |
||
|
Employed Jobless Lawyer Student Teacher Others |
18 247 3 21 16 23 |
5.5 75.3 0.9 6.4 4.9 7 |
|
Marital Status |
||
|
Married Single |
283 43 2 |
86.3 13.1 0.6 |
|
Chief Complain |
||
|
Abnormal Menstruation Cold Intolerance Hair Loss Incidental Neck Pain Neck Swelling Neck Weakness Others |
19 6 5 81 37 18 146 16 |
5.8 1.8 1.5 24.7 11.3 5.5 44.5 4.6 |
|
Treatment |
||
|
1/week 2/week Daily |
100 119 109 |
30.5 36.3 33.2 |
| TSH: Thyroid stimulating hormone, SD: Standard deviation | ||
The median age was similar across the three groups, with 42.0 years (IQR 13.5) in the once-weekly group, 40.0 years (IQR 16.0) in the twice-weekly group, and 43.0 years (IQR 23.0) in the daily group (p = 0.061). Females predominated in all groups, accounting for 98% of the once-weekly group, 97.5% of the twice-weekly group, and 81.7% of the daily group, with a statistically significant difference (p < 0.001). Regarding occupation, the majority were jobless across all groups, but the daily group had a higher proportion of employed participants (9.2%) compared with the weekly groups (p < 0.001) (Table 2).
|
Variables |
Treatment |
P-value | ||
|
1/week (n=100) |
2/week (n=119) |
Daily (n=109) |
||
|
Age, median (IQR) |
42.0 (13.5) |
40.0 (16.0) |
43.0 (23.0) |
0.061 |
|
Sex |
|
|
|
<0.001
|
|
Female |
98 (98.0%) |
116 (97.5%) |
89 (81.7%) |
|
|
Male |
2 (2.0%) |
3 (2.5%) |
20 (18.3%) |
|
|
Marital Status |
|
|
|
|
|
Married |
88 (88.0%) |
95 (79.8%) |
100(91.7%) |
0.012 |
|
Single |
10 (10.0%) |
24 (20.2%) |
9 (8.3%) |
|
|
Widow |
2 (2.0%) |
0 (0.0%) |
0 (0.0%) |
|
|
Chief Complain |
|
|
|
|
|
Abnormal Menstruation |
7 (7.0%) |
8 (6.7%) |
4 (3.7%) |
<0.001 |
|
Cold Intolerance |
0 (0.0%) |
4 (3.4%) |
2 (1.8%) |
|
|
Hair Loss |
2 (2.0%) |
1 (0.8%) |
2 (1.8%) |
|
|
Incidental |
5 (5.0%) |
6 (5.0%) |
70 (64.2%) |
|
|
Neck Pain |
15 (15.0%) |
17 (14.3%) |
5 (4.6%) |
|
|
Neck Swelling |
6 (6.0%) |
9 (7.6%) |
3 (2.8%) |
|
|
Neck Weakness |
59 (59.0%) |
69 (58.0%) |
18 (16.5%) |
|
|
Others |
6 (6.0%) |
5 (4.2%) |
5 (4.6%) |
|
|
Occupation |
|
|
|
|
|
Employed |
2 (2.0%) |
6 (5.0%) |
10 (9.2%) |
<0.001 |
|
Jobless |
79 (79%) |
92 (77.3%) |
76 (69.7%) |
|
|
Lawyer |
2 (2.0%) |
1 (0.8%) |
0 (0.0%) |
|
|
Student |
8 (8.0%) |
10 (8.4%) |
3 (2.8%) |
|
|
Teacher |
7 (7.0%) |
7 (5.9%) |
2 (1.8%) |
|
|
Others |
2 (2.0%) |
3 (2.5%) |
18 (16.5%) |
|
| IQR: Interquartile range | ||||
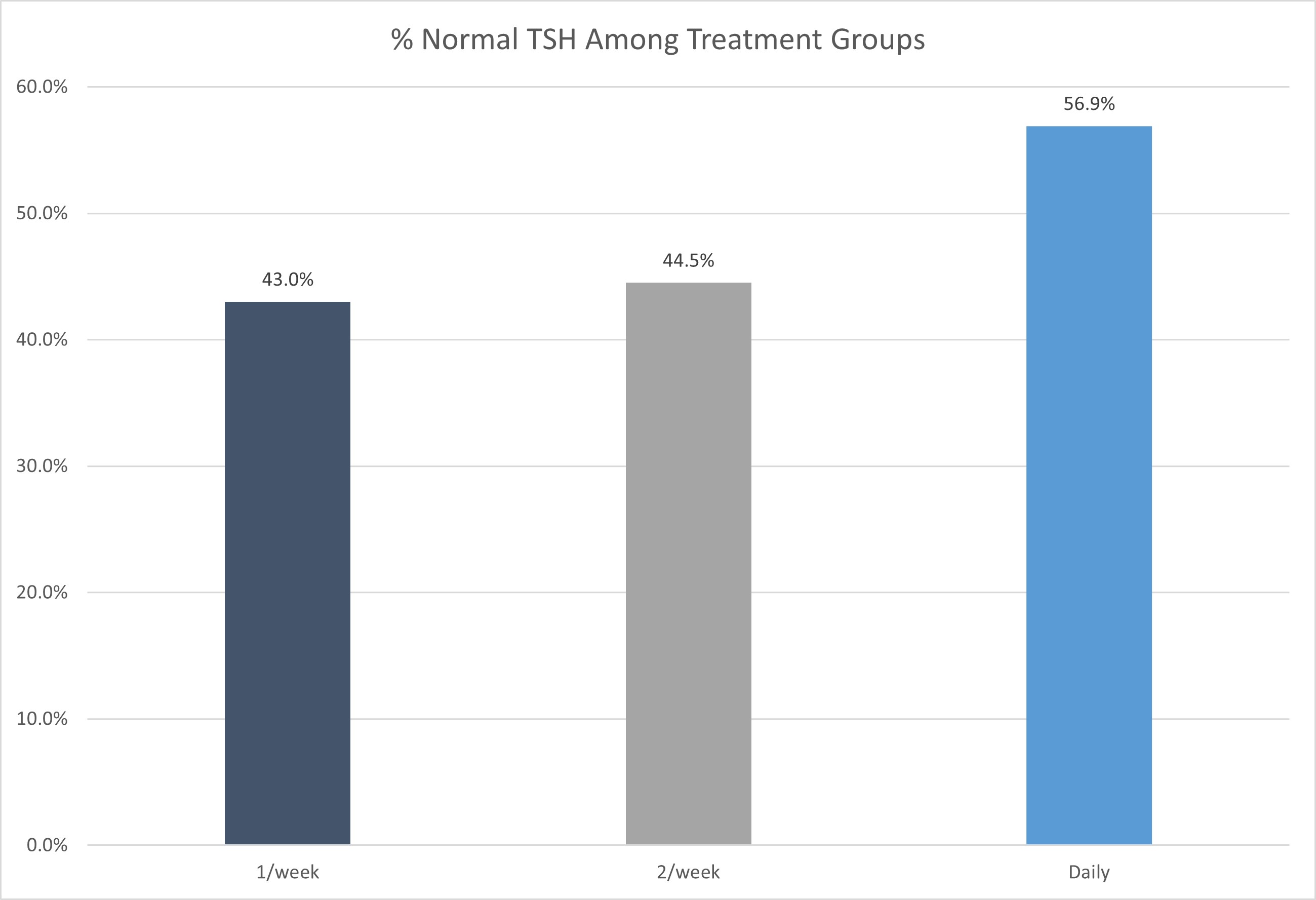
Before thyroxine therapy, in the once-weekly regimen group, the median value of TSH was 9.2 μIU/mL (IQR 6.8 μIU/mL), in the twice-weekly regimen group the level was 9.1 μIU/mL (IQR 7.3 μIU/mL), and in the standard daily dose group the median level was 15.4 (IQR 23.1 μIU/mL). After thyroxine intake and upon follow-up after six months, the TSH level decreased to 4.0 μIU/mL (IQR 3.7 μIU/mL), 4.2 μIU/mL (IQR 5.1 μIU/mL) and 4.5 μIU/mL (IQR 4.9 μIU/mL) in the standard daily, once- and twice-weekly regimen group, respectively (Figure 1) (Table 3). The outcome was statistically insignificant between groups. After six months of follow-up, 56.9% of patients in the daily regimen group, 43.0% in the once-weekly group, and 44.5% in the twice-weekly group achieved TSH levels within the normal reference range (Figure 2).
|
Variables |
Treatment |
P-value | ||
|
1/week (n=100) |
2/week (n=119) |
Daily (n=109) |
||
|
First TSH, median (IQR) |
9.2 (6.8) |
9.1 (7.3) |
15.4 (23.1) |
<0.001 |
|
Second TSH, median (IQR) |
4.5 (4.9) |
4.2 (5.1) |
4.0 (3.7) |
0.349 |
|
TSH Range |
|
|
|
|
|
<0.4 |
6 (6.0%) |
8 (6.7%) |
5 (4.6%) |
0.276 |
|
0.4 - 4.2 |
43 (43.0%) |
53 (44.5%) |
62 (56.9%) |
|
|
>4.2 |
51 (51.0%) |
58 (48.7%) |
42 (38.5%) |
|
| TSH: Thyroid stimulating hormone, IQR: Interquartile range | ||||
Compared to the daily treatment group, patients in the once-weekly group had an odds ratio (OR) of 0.659 (95% CI: 0.310–1.398, p = 0.277), and those in the twice-weekly group had an OR of 0.763 (95% CI: 0.363–1.602, p = 0.474), indicating no statistically significant difference in achieving normal TSH between the treatment regimens. Gender was not a significant predictor; males had an OR of 1.845 (95% CI: 0.439–7.751, p =0.403) compared to females. Age and baseline TSH similarly did not significantly influence the likelihood of achieving normal TSH (OR = 0.997, p = 0.801 and OR = 0.995, p = 0.317, respectively) (Table 4).
|
Parameters |
B (S.E) |
Exp (B) (OR) |
95% CI |
P-value |
|
Treatment Group Daily* 1/week 2/week |
-0.418 (0.384) -0.271 (0.379) |
1 0.659 0.763 |
0.310-1.398 0.363-1.602 |
0.277 0.474 |
|
Age (Years) |
-0.003 (0.010) |
0.997 |
0.978-1.017 |
0.801 |
|
Gender Female* Male |
0.612 (0.732) |
1 1.845 |
0.439-7.751 |
0.403 |
|
First TSH |
-0.005 (0.005) |
0.995 |
0.985-1.005 |
0.317 |
|
Occupation Employed* Jobless Lawyer Student Teacher Others |
0.497 (0.568) 0.201 (1.367) 0.196 (0.795) 0.267 (0.758) -0.138 (0.788) |
1 1.643 1.223 1.217 1.306 0.871 |
0.540-5.002 0.084-17.827 0.256-5.780 0.296-5.770 0.186-4.084 |
0.382 0.883 0.805 0.724 0.861 |
|
Marital Status Married Single Widow |
-0.249 (0.434) 0.104 (1.496) |
1 0.779 1.109 |
0.333-1.825 0.059-20.814 |
0.566 0.945 |
Discussion
Hypothyroidism can often occur as a result of thyroiditis or thyroidectomy to remove part of or the entire thyroid tissue [4-6]. The standard treatment for hypothyroidism involves daily administration of thyroxine, a synthetic form of the thyroid hormone. However, emerging evidence suggests that a weekly thyroxine regimen may offer several advantages in terms of patient convenience, treatment adherence, and potentially improved clinical outcomes [7]. Noncompliance with thyroxine is the most prevalent cause of poor hypothyroidism management, which is linked to the discomfort of taking the drug when fasting, waiting 60 minutes for the next meal or beverage, and avoiding other medications that may interfere with thyroxine absorption [8]. The feasibility of weekly thyroxine dosing lies in the pharmacokinetics of levothyroxine. It has a long half-life, with stable levels maintained in the bloodstream for several weeks. Additionally, the availability of thyroxine formulations that allow for extended release further supports the feasibility of weekly dosing [9].
One of the primary advantages of weekly thyroxine is the potential for enhanced patient convenience and improved treatment adherence. Daily medication regimens can be challenging for patients to adhere to consistently, leading to suboptimal management of hypothyroidism. Weekly thyroxine simplifies the dosing schedule, reducing the burden of daily medication intake [10]. Studies have shown that non-adherence to daily thyroxine therapy is common and can result in inadequate control of thyroid function. By reducing the frequency of dosing, weekly thyroxine may address the issue of non-adherence and improve the effectiveness of treatment in achieving target thyroid hormone levels and overall clinical outcomes [11].
There have been very few studies comparing daily versus weekly treatment of thyroxine in hypothyroid patients globally. Therefore, there is a crucial need to expand the current body of litrerature on this treatment strategy. According to one study, in today's world of busy lifestyles, when it is difficult for patients to take thyroxine on a strict schedule, once-weekly thyroxine administration gives an alternate option for treating hypothyroidism, particularly in patients whose compliance is a big concern [12]. Bornschein et al. found comparable results between daily and weekly dosing, with no hyperthyroidism in patients with weekly regimens [10]. Rangan et al. demonstrated in a case series of two patients that once-weekly thyroxine is an alternate treatment approach for noncompliant patients and remarked that once-weekly thyroxine is a safe treatment regimen [11]. Another study found that when compared to a daily dosage of thyroxine, once weekly thyroxine is an effective and safe long-term treatment option for individuals with poor management of hypothyroidism or apparent thyroxine resistance. With directly monitored once-weekly thyroxine, approximately three-quarters of such individuals are able to achieve TSH normalization [8]. According to Chiu et al., weekly thyroxine administration results in less suppression and greater overall TSH levels while keeping below the normal reference range as specified by worldwide treatment recommendations. It may be a viable option for hypothyroid individuals, especially if compliance is an issue [13].
Concerns have also been expressed that taking a big dose of once-weekly thyroxine may result in increased supraphysiologic levels of thyroxine in the first few days, which may have an unfavorable effect on cardiovascular function. It is also believed that by the sixth day of thyroxine administration, the efficacy of once-weekly thyroxine would have worn off, resulting in the recurrence of hypothyroid symptoms and swings in TSH levels [14]. Grebe et al. showed that, while weekly treatment was well tolerated, thyroid function tests showed significant hypothyroidism with an increase in TSH and a decrease in thyroxine before the next weekly prescription [15]. A meta-analysis of four trials including 294 participants evaluated the effect of once weekly thyroxine on TSH after 6 weeks of treatment. After 6 weeks of therapy, once weekly thyroxine patients had considerably greater serum TSH than standard daily thyroxine patients [14]. The results of the current study showed that once weekly and twice weekly thyroxine were almost equally effective as standard daily thyroxine in achieving and maintaining normal thyroid function. There were no significant differences between the three treatment groups.
This study has several limitations, including relatively small group sizes, a single-center design, and a short follow-up period of six months. Despite these limitations, the findings provide supportive evidence that may have implications for current clinical practice regarding thyroxine administration. Future research involving larger, multicenter cohorts with longer follow-up periods is warranted to validate and expand upon these results.
Conclusion
The comparison of once-daily, once-weekly, and twice-weekly thyroxine administration highlights the potential benefits of less frequent dosing for hypothyroidism management. While all regimens appear to maintain comparable efficacy and safety, the convenience and potential for improved adherence associated with less frequent dosing regimens are notable. However, patient response to weekly thyroxine can vary, and some individuals may require more frequent administration or may not be suitable candidates for weekly therapy. Additionally, infrequent dosing carries the risk of missed doses, which could compromise treatment effectiveness. Therefore, close monitoring of thyroid function and individualized dose adjustments are essential to optimize outcomes. Long-term studies are needed to evaluate the sustained efficacy, safety, and patient satisfaction with weekly thyroxine regimens. Further research comparing different thyroxine formulations for weekly dosing and assessing their impact on specific populations, such as pregnant women or patients with comorbidities, would be valuable.
Declarations
Conflicts of interest: The authors have no conflicts of interest to disclose.
Ethical approval: Ethical approval for this study (Ethical Committee No: 95) was provided by the Ethical Committee of School of Medicine-University of Sulaimani.
Patient consent (participation and publication): Written informed consent was obtained from all patients and/or their legal guardians for participation in this study and for the publication of any accompanying images, clinical information, and other data included in the manuscript.
Source of Funding: Smart Health Tower.
Role of Funder: The funder remained independent, refraining from involvement in data collection, analysis, or result formulation, ensuring unbiased research free from external influence.
Acknowledgements: None to be declared.
Authors' contributions: AMS and SFA were major contributors to the conception of the study, as well as to the literature search for related studies. MNH, SHH and HAH were involved in the literature review and the writing of the manuscript. ASM, MMA, HMZ, YAS, SHA, HOB, MAA and SHA were involved in the literature review, the design of the study, the critical revision of the manuscript, and the processing of the tables. AMS and MNH confirm the authenticity of all the raw data. All authors have read and approved the final manuscript.
Use of AI: AI was not used in the drafting of the manuscript, the production of graphical elements, or the collection and analysis of data.
Data availability statement: The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
- Gaitonde DY, Rowley KD, Sweeney LB. Hypothyroidism: an update. South African Family Practice. 2012;54(5):384-90. doi:N/A
- Lips DJ, Van Reisen MT, Voigt V, Venekamp W. Diagnosis and treatment of levothyroxine pseudomalabsorption. Neth J Med. 2004;62(4):114-8. doi:N/A
- Walker JN, Shillo P, Ibbotson V, Vincent A, Karavitaki N, Weetman AP, et al. A thyroxine absorption test followed by weekly thyroxineadministration: a method to assess non-adherence to treatment. European Journal of Endocrinology. 2013;168(6):913-7. doi:10.1530/EJE-12-1035
- Muhialdeen AS, Baba HO, Salih AM, Saeed YA, Abdullah IY, Qaradakhy AJ, et al. Redo thyroidectomy: A modified technique to eliminate complications. Barw Medical Journal. 2023;1(2). doi:10.58742/bmj.v1i2.27
- Salih AM, Kakamad FH, Rawezh QS, Masrur SA, Shvan HM, Hawbash MR, et al. Subacute thyroiditis causing thyrotoxic crisis; a case report with literature review. International journal of surgery case reports. 2017;33(1):112-4. doi:10.1016/j.ijscr.2017.02.041
- Salih AM, Baba HO, Ahmed MM, Kakamad FH, Hassan HA, Hassan MN, et al. Modified thyroidectomy: 4 techniques to prevent recurrent laryngeal nerve injury and postoperative hypocalcaemia. IJS Short Reports. 2022;7(2):e45. doi:10.1097/SR9.0000000000000045
- Chiovato L, Magri F, Carlé A. Hypothyroidism in context: where we’ve been and where we’re going. Advances in therapy. 2019;36:47-58. doi:10.1007/s12325-019-01080-8
- Jayakumari C, Nair A, Puthiyaveettil Khadar J, Das DV, Prasad N, Jessy SJ, et al. Efficacy and safety of once-weekly thyroxine for thyroxine-resistant hypothyroidism. Journal of the Endocrine Society. 2019;3(12):2184-93. doi:10.1210/js.2019-00212
- Colucci P, Yue CS, Ducharme M, Benvenga S. A review of the pharmacokinetics of levothyroxine for the treatment of hypothyroidism. European endocrinology. 2013;9(1):40. doi:10.17925/EE.2013.09.01.40
- Bornschein A, Paz-Filho G, Graf H, Carvalho GA. Treating primary hypothyroidism with weekly doses of levothyroxine: a randomized, single-blind, crossover study. Arquivos Brasileiros de Endocrinologia & Metabologia. 2012;56:250-8. doi:10.1590/S0004-27302012000400006
- Rangan S, Tahrani AA, Macleod AF, Moulik PK. Once weekly thyroxine treatment as a strategy to treat non-compliance. Postgraduate Medical Journal. 2007;83(984):e3-. doi:10.1136/pgmj.2007.060244
- Rajput R, Pathak V. The effect of daily versus weekly levothyroxine replacement on thyroid function test in hypothyroid patients at a tertiary care centre in Haryana. European Thyroid Journal. 2017;6(5):250-4. doi:10.1159/000477348
- Chiu HH, Larrazabal Jr R, Uy AB, Jimeno C. Weekly versus daily levothyroxine tablet replacement in adults with hypothyroidism: a meta-analysis. Journal of the ASEAN Federation of Endocrine Societies. 2021;36(2):156. doi:10.15605/jafes.036.02.07
- Dutta D, Jindal R, Kumar M, Mehta D, Dhall A, Sharma M. Efficacy and safety of once weekly thyroxine as compared to daily thyroxine in managing primary hypothyroidism: A systematic review and meta-analysis. Indian Journal of Endocrinology and Metabolism. 2021;25(2):76. doi:10.4103/ijem.IJEM_789_20
- Grebe SK, Cooke RR, Ford HC, Fagerström JN, Cordwell DP, Lever NA, et al. Treatment of hypothyroidism with once weekly thyroxine. The Journal of Clinical Endocrinology & Metabolism. 1997;82(3):870-5. doi:10.1210/jcem.82.3.3830

This work is licensed under a Creative Commons Attribution 4.0 International License.

