Management of Lower Limb Varicose Veins Using Endovenous Laser Ablation, Micro-Phlebectomy, and Sclerotherapy Using Multimodal Analgesia
Abstract
Introduction
Previously, the conventional surgical procedure of high-ligation and saphenous stripping was commonly used to treat varicose veins (VVs). However, contemporary advancements have led to the rapid evolution of VV management. This study shares a single center's experience in treating patients with lower limb VVs through endovenous laser ablation in combination with phlebectomy and sclerotherapy using multimodal analgesia.
Methods
This case series study included consecutive patients diagnosed with lower limb VVs. The inclusion criteria encompassed VVs categorized from score C1 to C6 clinical, etiologic, anatomic, and pathophysiological (CEAP), saphenofemoral incompetence, and patients aged between 18 and 75.
Results
A total of 153 patients were enrolled. The majority were female (73.0%), resulting in a female-to-male ratio of 2.73:1. The age of patients ranged from 18 to 73 years, with a mean age of 40.8 ± 11.7 years. Regarding post-procedural complications, wounds developed in 25 patients (16.3%), making it the most common complication, while thrombophlebitis occurred in 15 cases (9.8%), skin discoloration in nine cases (5.9%), and recanalization and DVT each in a case (0.7%). Due to extensive varicose veins, 31 patients (20.0%) required a sclerotherapy session six weeks after the operation. Patients could return to routine daily activities within 4 to 10 hours. Overall, the patient satisfaction rate (complete and partial) was 85%. Only a case of recurrence (0.7%) was reported after a one-year follow-up.
Conclusion
Endovenous laser ablation, in combination with phlebectomy and sclerotherapy using multimodal analgesia, may yield a satisfactory outcome in patients with moderate to severe VVs.
Introduction
Varicose veins (VVs) are abnormally twisted and dilated blood vessels, typically located in the lower limbs. They originate from damaged or faulty venous valves, which may subsequently give rise to painful swelling and the potential formation of blood clots [1]. It is the most commonly encountered among vascular diseases, affecting up to one-third of the population and profoundly impacting the quality of life [2]. Increased age, female gender, multiparity, obesity, a history of deep venous thrombosis (DVT), and engagement in occupations involving extended periods of standing are all recognized as significant risk factors associated with the onset of VVs [3]. Historically, VVs were often viewed as a cosmetic problem, and patient preferences largely influenced treatment decisions. However, advancements in medical imaging, particularly duplex ultrasonography, revolutionized the understanding of VVs by providing a more precise assessment of venous reflux and allowing healthcare professionals to accurately diagnose the underlying venous insufficiency contributing to VVs [4]. Previously, the conventional surgical procedure of high-ligation and saphenous stripping was commonly used for the treatment of VVs. However, contemporary advancements have led to the rapid evolution of VV management, offering minimally invasive interventions such as radiofrequency (RFA), laser ablations, foam, liquid sclerotherapy, and microphlebectomy [5]. Endovenous laser ablation (EVLA) uses laser energy to occlude impaired veins, rerouting blood circulation toward healthier venous pathways. Microphlebectomy presents another alternative therapeutic modality involving the surgical removal of superficial veins via small puncture incisions. Sclerotherapy entails the injection of a sclerosing agent into afflicted veins, resulting in their closure and redirection of blood flow [6]. This study aims to share the experience of a single center in treating patients with lower limb VVs through EVLA in combination with phlebectomy and sclerotherapy under multimodal analgesia. The study avoided citing suspicious data by checking for predatory behavior among the referenced studies [7].
Methods
Study design
The study was a single-center case series encompassing consecutive patients diagnosed with lower limb VVs and treated at the Thoracic and Vascular Surgery Department of Smart Health Tower from January 2020 to September 2023. Patients provided consent to participate in the study and to authorize the publication of any related data.
Data collection
Following data de-identification, the necessary information was retrospectively gathered from patients' profiles within the department's database. This included patient demographics, chief complaint, clinical score, affected side, severity of the condition, ultrasound examination results, and treatment outcomes.
Eligibility criteria
The inclusion criteria encompassed VVs categorized from score C1 to C6 (clinical, etiologic, anatomic, and pathophysiological) (CEAP), presence of saphenofemoral incompetence, and patients aged between 18 and 75 years. The exclusion criteria comprised any prior treatment of VVs, suspicion or confirmation of DVT or occlusion, contraindications to anesthesia, and refusal to undergo the treatment procedure.
Intervention
In the pre-operative phase, approximately 30 minutes before the operation, patients received a combination of medications, including pethidine (50 mg subcutaneously), ketorolac (30 mg intramuscularly), and ondansetron (8 mg), if there were no contraindications. In the operating theater, intravenous pethidine was administered after properly marking the varicose vein sites by injecting normal saline, patient positioning, and monitoring. This was followed by a slow tramadol infusion (100 mg) and paracetamol (1000 mg). Continuous administration of dexmedetomidine (100 –150 µg in 100 ml of normal saline) was initiated, with oxygen supplementation adjusted as necessary. Antiemetic drugs, aside from ondansetron, were administered during the procedure unless contraindicated. In rare cases of anxiety or the requirement for minimal sedation, fentanyl (50 µg), midazolam (1mg), or a combination of both were included.
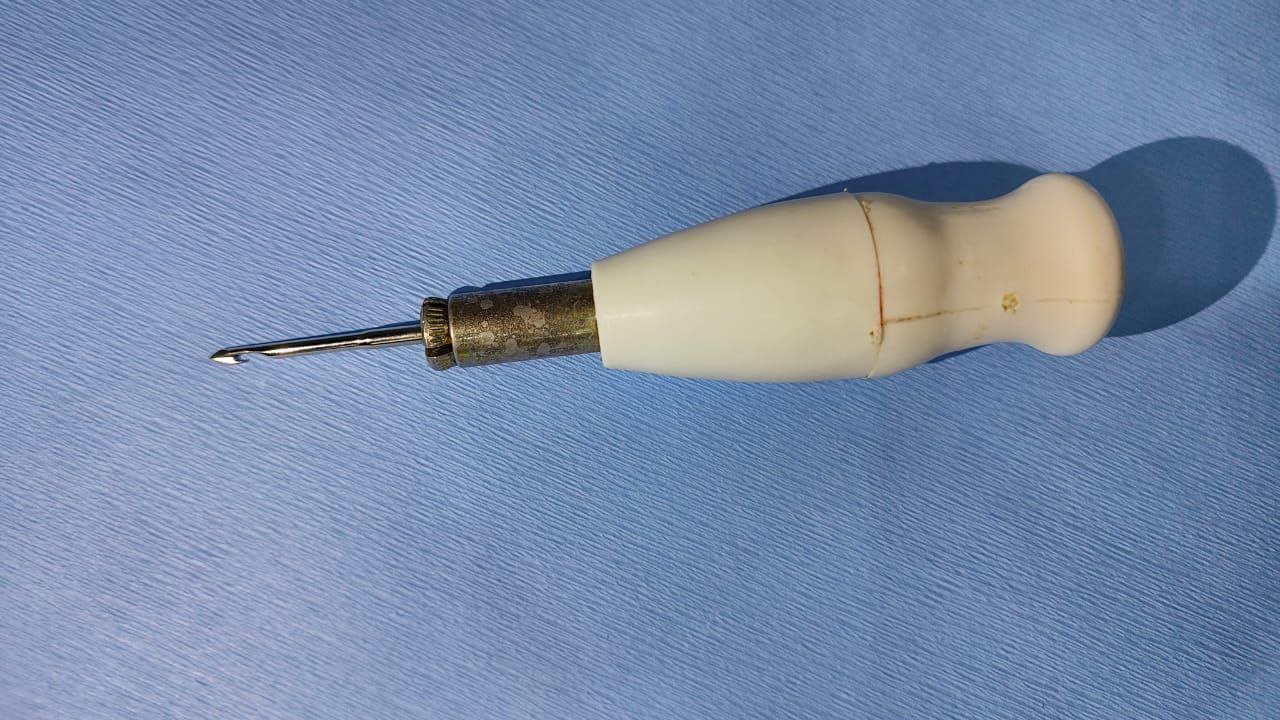
The EVLA procedure started with a Doppler ultrasound by a radiologist to guide a needle to access the great saphenous vein (GSV). Then, a guide wire was carefully inserted into the vein, followed by the placement of an introducer sheath, which might include a dilator. Just below knee level was the preferred entry point for the insufficient GSV due to its larger size, straight course, and lower risk of nerve injury. The laser (1470 nm) was inserted into the varicose vein after verifying the laser's tip position by observing the red standby light through the skin with a diameter between 200 and 600 mm (dependent on the varicose vein and the laser parameters). The laser's settings were customized as necessary, and it was carefully withdrawn through the vein using a technique suited to the specific situation. The laser power was calibrated according to the vein size, with a minimum setting of 42 watts. The power was determined by multiplying the vein diameter by a factor of 7. After major vein ablation, micro-avulsion was done for the visible varicose veins using a particular instrument (Drosh) (Figure 1). The reticular and telangiectasia were injected with a foamy solution consisting of two ml of polidocanol and eight ml of atmospheric air (1:4) as the sclerosing agent.
Statistical analysis
The data organization was conducted using Microsoft Excel 2019. Descriptive analysis was performed using the Statistical Package for the Social Sciences (SPSS) Version 25 for qualitative data synthesis. The data were presented as medians, means, standard deviations, frequencies, percentages, and ranges.
Results
A total of 153 patients were enrolled in this study. The majority were female (73.0%), resulting in a female-to-male ratio of 2.73:1. The age of patients ranged from 18 to 73 years, with a mean age of 40.8 ± 11.7 years. Over half of the cases were overweight (54.9%), and the mean BMI was 26.3 ± 4.2. The major chief complaint was pain (17.7%), followed by swelling (15.0%) and lower limb discoloration (5.2%). The disease was asymptomatic in 59.5% of the cases. The disease presented as VVs (C2) in most cases (73.9%), although 21 (13.7%) presented with reticular veins (C1) and 10 (6.5%) with telangiectasia (C1). Disease severity was moderate in over half of the cases (53.6%), followed by severe in 51 cases (33.3%). The majority of patients (61.4%) had bilateral lower limb involvement, while the remaining patients had unilateral involvement, with 22.2% affected in the left lower limb and 16.3% in the right lower limb. The mean diameters of the GSV undergoing treatment were 9 mm.
The mean reflux duration of the affected veins was 1.1 seconds, ranging from 0.6 to 2.5 seconds, with the procedure duration ranging from 45 to 220 minutes. Regarding post-procedural complications, wounds developed at the site of sclerosant injection in 25 patients (16.3%), making it the most common complication, while thrombophlebitis occurred in 15 cases (9.8%), skin discoloration in nine cases (5.9%), and recanalization and DVT each in a case (0.7%). The thrombophlebitis cases were treated with an anti-inflammatory agent. Wounds healed with proper dressing within two to three weeks. Due to extensive VVs, 31 patients (20.0%) required sclerotherapy six weeks after the operation. Additionally, all instances of skin discoloration resolved spontaneously. Patients could return to routine daily activities within 4 to 10 hours. Overall, 54.3% of the patients were completely satisfied with the outcome. Meanwhile, 30.7% were partially satisfied, and 15.0% were not satisfied with the procedure. Only a case of recurrence was reported during the one-year follow-up (Table 1).
|
Variables |
Frequency / Percentage |
|
Demographics |
|
|
Age range (median, mean ± SD), years |
18 – 73 (40, 40.8 ± 11.7) |
|
BMI (mean± SD), kg/m2 Underweight Normal Overweight Obesity |
26.3 ± 4.2 3 (2.0%) 52 (34.0%) 84 (54.9%) 14 (9.1%) |
|
Gender Male Female |
41 (27.0%) 112 (73.0%) |
|
Chief complaint Pain Swelling Lower limb discoloration Itching Extensive varicose vein impending rupture |
27 (17.7%) 23 (15.0%) 8 (5.2%) 4 (2.6%) 91 (59.5%) |
|
CEAP classification C1 C2 C3 C4 C5 C6 |
21 (13.7%) 113 (73.9%) 8 (5.2%) 6 (3.9%) 5 (3.3%) 0 (0.0%) |
|
Severity status Mild Moderate Severe |
20 (13.1%) 82 (53.6%) 51 (33.3%) |
|
Affected site Right lower limb Left lower limb Both lower limbs |
25 (16.3%) 34 (22.2%) 94 (61.4%) |
|
Reflux duration (seconds), mean (range) |
1.1 (0.6-2.5) |
|
Diameter of GSV (mm), mean (range) |
9 (6-22) |
|
Operation time (minutes), mean (range) |
70 (45-220) |
|
Returning to routine daily activity (hours), mean (range) |
6 (4-10) |
|
Satisfaction level Completely satisfied Partially satisfied Not satisfied |
47 (30.7%) 23 (15.0%) |
|
Post-procedure complications Wounds at the site of injections Thrombophlebitis Skin discoloration Recanalization Deep vein thrombosis |
25 (16.3%) 15 (9.8%) 9 (5.9%) 1 (0.7%) 1 (0.7%) |
|
Post laser injection (sclerotherapy) Yes No |
122 (80.0%) |
|
Recurrence |
1 (0.7%) |
Discussion
The VVs represent a prevalent condition, with occurrence rates typically ranging from 29.5% to 39.0% in women and 10.4% to 23.0% in men [1]. Annually, the condition manifests in approximately 2.6% of women and 1.9% of men. Its prevalence consistently rises with age, a trend often associated with increased height, weight, and body mass [1,8]. Chronic venous disease exacerbates the severity of symptoms, progressing from telangiectasia, characterized by the formation of threadlike patterns on the skin (referred to as spider veins), to VVs. This progression often imposes a substantial negative impact on the patient's quality of life [9]. In the current study, consistent with the genuine literature, females were predominantly affected, with a female-to-male ratio of 2.73:1. The mean age of patients, 40.8 years, aligns with previous findings [1,8]. The primary manifestation of the disease was VVs in the majority of cases (73.9%), indicating significant disease progression. Among the cases, the severity was moderate in 53.6% and severe in 33.3%.
Aligned with technological advancements, continual investigation has been undertaken to explore therapeutic approaches for treating VVs through endovenous methodologies [10]. A pivotal milestone occurred in 2001 when Navarro et al. reported the inaugural utilization of thermal endovenous ablation employing an 810 nm diode laser [11]. Subsequently, a consistent evolution in laser technology has ensued, accompanied by many studies employing diverse wavelengths and laser modalities [10,12,13]. At present, the Food and Drug Administration (FDA) has approved lasers of various wavelengths, including 810, 940, 980, and 1470 nm diode lasers, alongside 1319 and 1320 nm neodymium-doped yttrium aluminum garnet (Nd: YAG) lasers. Simultaneously, the progression of laser technology has stimulated research into thermal ablation techniques for the GSV using radiofrequency energy. The FDA endorsement for the application of radiofrequency energy in endovenous ablation procedures was granted in 1999 [10]. In 2002, Weiss et al. published the initial cases wherein patients underwent thermal ablation employing radiofrequency energy [14]. The current clinical practice guidelines advocate for ablation (EVLA and RFA) as the primary treatment for superficial venous insufficiency while recommending phlebectomy or sclerotherapy for addressing varicosities [15]. In the present study, EVLA (1470 nm) was employed in combination with phlebectomy and sclerotherapy to manage VVs in 153 patients.
A meta-analysis of 119 studies found success rates of 94% for EVLA and 84% for RFA from data on 12,320 legs [16]. Puggioni et al. reported one-month follow-up success rates of 100% for EVLA and 96% for RFA [17]. Bozoglan et al. reported no significant complications such as DVT, pulmonary embolism, or skin burns in either EVLA or RFA. Minor complications included induration (20.7% in EVLA and 31% in RFA), ecchymosis (31% in EVLA and 27.6% in RFA), and edema (27.6% in EVLA and 65.5% in RFA). They claimed that most minor complications, such as hematoma and ecchymosis, were attributed to the use of tumescent anesthesia rather than the procedures themselves. They reported a recanalization rate of 6.8% in the RFA group, while no instances of recanalization were noted in the EVLA group. Patient satisfaction levels were significantly higher with EVLA at 51.7% compared to the 31.0% satisfaction rate observed for RFA. Only 17.2% of patients reported satisfaction with both procedures. Individuals in the EVLA group typically returned to daily activities within 0.9 days, while those in the RFA group took an average of 1.3 days to resume regular activities. The mean duration of procedures was 31.2 minutes for EVLA and 32.7 minutes for RFA [10]. Another study involving 148 patients undergoing EVLA reported pain in over 50% of patients, hematoma in 40.5%, superficial vein thrombosis in 6.8%, induration in 6.8%, hyperpigmentation in 3.4%, infection and dysesthesia in less than 2%, and nerve damage occurring in less than 1% of cases [18]. Additionally, a meta-analysis reported the incidence of thrombophlebitis and hematoma at 4.9% and 4.4%, respectively [19]. Kawai et al. performed EVLA with and without phlebectomy and found hematoma in 26.6% of cases with phlebectomy and 23.2% of cases without phlebectomy. They reported no instances of DVT [15]. Because sclerotherapy plays a significant role in managing and diminishing the appearance of VVs, which have reached a severe stage [1], they needed additional sclerotherapy in 8 cases (3.2%) in the phlebectomy group and 26 cases (3.7%) in the non-phlebectomy group. The operation time ranged from 27 to 40 minutes in the EVLA with the phlebectomy group and 19 to 31 minutes in the counterpart group. Recanalization was observed in four cases (1.6%) in the EVLA with the phlebectomy group and in 25 cases (3.6%) in the latter group [15]. In this study, developing wounds was the most prevalent complication (16.3%), followed by thrombophlebitis (9.8%) and skin discoloration (5.9%). Thrombophlebitis was treated with an anti-inflammatory agent, skin discoloration resolved spontaneously, and wounds healed within a few weeks with dressing. The duration of the operation in the present study ranged from 45 to 220 minutes, with a mean of 70 minutes. The recanalization rate (0.7%) was lower than the rate reported by Kawai et al. [15] but higher than that reported by Bozoglan et al [10]. Patients returned to daily activities within 4 to 10 hours, and the overall treatment satisfaction (partial and complete) reached 85%, surpassing Bozoglan et al.'s [10]. There was a case of DVT, and sclerotherapy was required in 20% of cases due to the severity of the disease.
Regarding the working principle, EVLA enables veins to absorb energy for heat generation, leading to vein obliteration. The energy utilized during the procedure significantly impacts the outcome. It has been discovered that energy delivery directly influences recurrence, with lower energy levels yielding poorer outcomes than higher energy levels [20]. The recurrence rate for up to 10 years was found to be 66% in EVLA, and 36% of the patients needed reintervention [21]. To mitigate the risk of recurrence, a laser wavelength of 1470 nm was employed in the procedures of the current study. After one year of follow-up, only a case of recurrence was reported. This study has some drawbacks, including a retrospective design that means crucial data may be overlooked for discussion and a short follow-up period to properly indicate the recurrence rate.
Conclusion
Endovenous laser ablation, in combination with phlebectomy and sclerotherapy using multimodal analgesia, may yield a satisfactory outcome in patients with moderate to severe VVs.
Declarations
Conflicts of interest: The authors have no conflicts of interest to disclose.
Ethical approval: Not applicable.
Patient consent (participation and publication): Patients provided consent to participate in the study and to authorize the publication of any related data.
Source of Funding: Smart Health Tower.
Role of Funder: The funder remained independent, refraining from involvement in data collection, analysis, or result formulation, ensuring unbiased research free from external influence.
Acknowledgements: None to be declared.
Authors' contributions: FHK was a major contributor to the study's conception and to the literature search for related studies. SHT, AAM, and RJR were the radiologists who provided access to the cases. HOA, BAA, and MNH were involved in the literature review, study design, and writing of the manuscript. FEF, KAS, and BYA were the anesthesiologists who anaesthetized the cases. DHMS, FJA, NSS, PMK, BAA, AMM and SJJ were involved in the literature review, the study's design, the critical revision of the manuscript, and the table processing. All authors have read and approved the final version of the manuscript.
Use of AI: ChatGPT-3.5 was used to assist in language editing and improving the clarity of the manuscript. All content was reviewed and verified by the authors. Authors are fully responsible for the entire content of their manuscript.
Data availability statement: Not applicable.
References
- Gawas M, Bains A, Janghu S, Kamat P, Chawla P. A comprehensive review on varicose veins: preventive measures and different treatments. Journal of the American Nutrition Association. 2022;41(5):499-510, doi:10.1080/07315724.2021.1909510
- Yang L, Wang X, Wei Z, Zhu C, Liu J, Han Y. The clinical outcomes of endovenous microwave and laser ablation for varicose veins: A prospective study. Surgery. 2020;168(5):909-14, doi:10.1016/j.surg.2020.06.035
- Shadrina AS, Sharapov SZ, Shashkova TI, Tsepilov YA. Varicose veins of lower extremities: Insights from the first large-scale genetic study. PLoS Genet. 2019;15(4): 1008110. doi:10.1371/journal.pgen.1008110
- Gloviczki P, Gloviczki ML. Guidelines for the management of varicose veins. Phlebology. 2012;27(1_suppl):2-9. doi:10.1258/phleb.2012.012s28
- Turaga A H. Endovenous Laser Ablation-Phlebectomy-Sclerotherapy Hybrid Treatment for Venous Insufficiency: A Case Report. Cureus. 2023;15(7): 42161. doi:10.7759/cureus.42161
- Licker M, Brandao-Farinelli E, Cartier V, Gemayel G, Christenson JT. Implementation of a fast-track-pathway including analgo-sedation with local anaesthesia for outpatient varicose vein surgery: a cohort study. Phlebology. 2013;28(8):418-425, doi:10.1258/phleb.2012.012074
- Kakamad FH, Abdalla BA, Abdullah HO, Omar SS, Mohammed SH, Ahmed SM et al. Lists of predatory journals and publishers: a review for future refinement. European Science Editing. 2024;50:e118119. doi:10.3897/ese.2024.e118119
- Ismail L, Normahani P, Standfield NJ, Jaffer U. A systematic review and meta-analysis of the risk for development of varicose veins in women with a history of pregnancy. Journal of Vascular Surgery: Venous and Lymphatic Disorders. 2016;4(4):518-24, doi:10.1016/j.jvsv.2016.06.003
- Tan MK, Sutanto SA, Onida S, Davies AH. The relationship between vein diameters, clinical severity, and quality of life: a systematic review. European Journal of Vascular and Endovascular Surgery. 2019;57(6):851-7. doi:10.1016/j.ejvs.2019.01.024
- Bozoglan O, Mese B, Eroglu E, Erdogan MB, Erdem K, Ekerbicer HC, et al. Comparison of endovenous laser and radiofrequency ablation in treating varicose veins in the same patient. Vascular and Endovascular Surgery. 2016;50(1):47-51, doi:10.1177/1538574415625813
- Navarro L, Min RJ, Boné C. Endovenous laser: a new minimally invasive method of treatment for varicose veins—preliminary observations using an 810 nm diode laser. Dermatologic surgery. 2001;27(2):117-22. doi:10.1046/j.1524-4725.2001.00134.x
- Vuylsteke ME, Thomis S, Mahieu P, Mordon S, Fourneau I. Endovenous laser ablation of the great saphenous vein using a bare fibre versus a tulip fibre: a randomised clinical trial. European journal of vascular and endovascular surgery. 2012;44(6):587-92. doi:10.1016/j.ejvs.2012.09.003
- Schwarz T, von Hodenberg E, Furtwängler C, Rastan A, Zeller T, Neumann FJ. Endovenous laser ablation of varicose veins with the 1470-nm diode laser. Journal of vascular surgery. 2010;51(6):1474-8. doi:10.1016/j.jvs.2010.01.027
- Weiss RA, Weiss MA. Controlled radiofrequency endovenous occlusion using a unique radiofrequency catheter under duplex guidance to eliminate saphenous varicose vein reflux: a 2-year follow-up. Dermatologic surgery. 2002;28(1):38-42. doi:10.1046/j.1524-4725.2002.01188.x
- Kawai Y, Sugimoto M, Aikawa K, Komori K. Endovenous laser ablation with and without concomitant phlebectomy for the treatment of varicose veins: a retrospective analysis of 954 limbs. Annals of Vascular Surgery. 2020;66:344-50. doi:10.1016/j.avsg.2019.12.025
- Van den Bos R, Arends L, Kockaert M, Neumann M, Nijsten T. Endovenous therapies of lower extremity varicosities: a meta-analysis. Journal of vascular Surgery. 2009;49(1):230-9. doi:10.1016/j.jvs.2008.06.030
- Puggioni A, Kalra M, Carmo M, Mozes G, Gloviczki P. Endovenous laser therapy and radiofrequency ablation of the great saphenous vein: analysis of early efficacy and complications. Journal of vascular surgery. 2005;42(3):488-93. doi:10.1016/j.jvs.2005.05.014
- Hamann SA, Timmer-de Mik L, Fritschy WM, Kuiters GR, Nijsten TE, Bos RR. Randomized clinical trial of endovenous laser ablation versus direct and indirect radiofrequency ablation for the treatment of great saphenous varicose veins. Journal of British Surgery. 2019;106(8):998-1004. doi:10.1002/bjs.11187
- He G, Zheng C, Yu MA, Zhang H. Comparison of ultrasound-guided endovenous laser ablation and radiofrequency for the varicose veins treatment: An updated meta-analysis. International journal of surgery. 2017;39:267-75. doi:10.1016/j.ijsu.2017.01.080
- Shrestha O, Basukala S, Thapa N, Karki S, Pant P, Paudel S. Endovenous laser ablation versus conventional surgery (ligation and stripping) for primary great saphenous varicose vein: a systematic review and meta-analysis. Annals of Medicine and Surgery. 2023;85(9):4509-19. doi:10.1097/MS9.0000000000001095
- Eggen CA, Alozai T, Pronk P, Mooij MC, Gaastra MT, Ünlü Ç, et al. Ten-year follow-up of a randomized controlled trial comparing saphenofemoral ligation and stripping of the great saphenous vein with endovenous laser ablation (980 nm) using local tumescent anesthesia. Journal of Vascular Surgery: Venous and Lymphatic Disorders. 2022;10(3):646-53. doi:10.1016/j.jvsv.2021.08.008

This work is licensed under a Creative Commons Attribution 4.0 International License.