Suture-Induced Tubo-Ovarian Abscess: A Case Report with Literature Review
Abstract
Introduction
Suture is an underreported cause for tubo-ovarian abscess (TOA) that can cause significant morbidity. This report describes a case of TOA arising from a silk suture three years after bilateral tubal ligation.
Case presentation
A 38-year-old woman with a history of tubal ligation presented with persistent pelvic pain and fever. Imaging revealed a suspicious left adnexal mass with features concerning for malignancy or abscess. Surgical exploration revealed a TOA adherent to surrounding structures, containing a retained silk suture from prior surgery. The abscess and suture were removed, and histopathology confirmed chronic inflammation without malignancy. The patient underwent additional procedures for thorough management, including polypectomy and contralateral tubal ligation.
Literature Review
A total of nine cases of TOAs and suture-induced abscesses were reviewed. Of these, seven were TOAs, six of which occurred postoperatively. Three cases developed following tubal ligation procedures. The abscesses ranged in size from 1 to 7.6 cm. The interval between the presumed inciting event and abscess detection varied widely, with one case presenting more than three decades after surgery. Isolated microorganisms included Escherichia coli, Streptococcus pyogenes, and Peptostreptococcus anaerobius. All patients underwent surgical intervention via various approaches, and several also received adjunctive antibiotic therapy.
Conclusion
Suture-induced TOA following sterilization may result in considerable morbidity, and surgical intervention may provide favorable outcomes.
Introduction
Pelvic inflammatory disease (PID) is a polymicrobial infection resulting from the ascent of pathogens from the cervix or vagina to the upper genital tract. It is most commonly caused by Chlamydia trachomatis and Neisseria gonorrhoeae, which together are responsible for approximately 60–75% of cases. Once these pathogens ascend, they can infect the endometrium, fallopian tubes, ovaries, and surrounding pelvic structures, triggering an inflammatory response [1].
A tubo-ovarian abscess (TOA) is a severe complication of PID, characterized by the formation of a purulent abscess involving the uterus, fallopian tubes, and ovaries [2]. This condition primarily affects women of reproductive age, with the highest incidence occurring in the fourth decade of life. Approximately 4.4% of sexually active women have a history of PID, placing them at increased risk for TOA development [3]. Given its non-specific clinical presentation, TOA can be challenging to diagnose, often requiring differentiation from other acute abdominal and pelvic conditions. The differential diagnosis includes ovarian torsion, ectopic pregnancy, appendicitis, gastroenteritis, constipation, and urinary tract infection, all of which can present with overlapping symptoms such as pelvic pain, fever, nausea, and gastrointestinal discomfort [2].
Although TOAs are commonly associated with PID, they can also develop from less common etiologies, such as the presence of surgical sutures. Reports of TOAs linked to surgical sutures remain scarce in the literature. This report highlights a unique case of a TOA that developed due to a silk suture three years after the patient had undergone bilateral tubal ligation, a procedure intended for permanent female sterilization. This case underscores the need for awareness of non-infectious etiologies in the differential diagnosis of TOAs, particularly in patients without a recent history of PID. The report was written according to the CaReL guidelines, and unreliable sources were excluded [4,5].
Case Presentation
Patient information
A 38-year-old female presented with a one-month history of worsening, persistent pelvic pain. Her medical history was unremarkable, and her surgical history included bilateral tubal ligation performed three years earlier.
Clinical findings
Physical examination revealed a high temperature, tenderness in the left suprapubic area, and the presence of an immobile pelvic mass upon palpation.
Diagnostic assessment
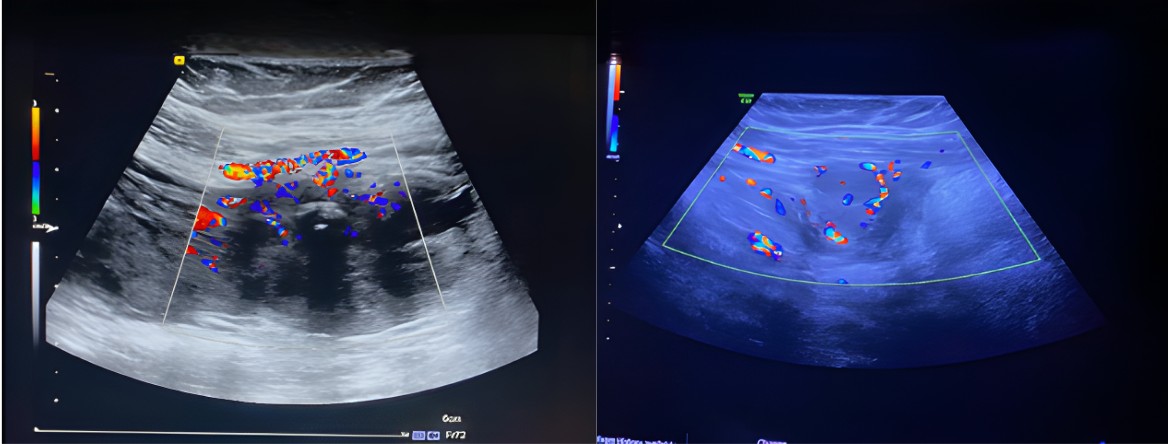
A pelvic ultrasound (US) showed a left-sided heterogeneous lesion measuring 44 x 30 mm. The mass was a vascular solid lesion with calcifications, exhibiting indistinct margins and evidence of invasion into the adjacent peritoneum and the left rectus abdominis muscle. Doppler imaging demonstrated high vascularity, with a score of 3-4. These characteristics were highly suspicious for a desmoid tumor or a primary peritoneal tumor; however, direct invasion of the left ovary could not be excluded (Figure 1). Computed tomography (CT) with IV contrast revealed a 6 x 4 x 3 cm, multilocular mass located in the left lower abdomen, arising from the left adnexa and attached to both the uterus and left ovary. The mass extended into the posterior aspect of the left rectus muscle. It was in proximity to the left inferior epigastric artery and a loop of small intestine, though no direct invasion was observed. Surrounding fat stranding raised the possibility of infection, such as a TOA, though malignancy could not be excluded. Mild pelvic free fluid was noted, and no suspicious lymph nodes were identified. The other abdominal organs, including the liver, spleen, pancreas, kidneys, and adrenal glands, appeared normal. The laboratory results revealed the following: Carcinoembryonic Antigen (CEA) was 0.471 ng/ml (normal range: 0-5 ng/ml), Cancer Antigen 125 (Ca125) was 33.6 IU/ml (normal range: <35 IU/ml), and Carbohydrate Antigen 19-9 (CA 19-9) was 5.73 IU/ml (normal range: <33 IU/ml), all of which fell within the normal reference ranges. Serum C-reactive protein (CRP) level was slightly elevated at 8.38 mg/L, above the normal range of <5.0 mg/L.
Therapeutic intervention
To ensure accurate diagnosis and appropriate management, consultations were held with oncology and gastrointestinal surgery specialists. After a thorough evaluation, an explorative laparoscopy was planned. During the procedure, a TOA was found, firmly adherent to the omentum and anterior abdominal wall. The abscess was carefully aspirated using suction, and a biopsy was taken for frozen section analysis. The preliminary histopathology report indicated inflammation and fibrosis, confirming the lesion's nature. As the surgery progressed, an unexpected finding was discovered: an unabsorbable silk suture embedded within the abscess. This suture, most likely a remnant from her previous procedure, was carefully excised along with the surrounding fibrotic tissue and sent for further histopathological analysis. To reduce the risk of recurrence, the contralateral fallopian tube was also removed and securely ligated. In addition to addressing the abscess and suture, a hysteroscopy and polypectomy were performed to ensure thorough treatment. The procedure was completed successfully, with all abscess material and pathological tissues removed. The histopathological examination revealed a hyperplastic endometrial polyp with background secretory changes consistent with progestin exposure, without evidence of atypia or malignancy. The left tubal mass showed chronic nonspecific salpingitis, and the attached omentum exhibited severe acute-on-chronic inflammation with fibrosis, consistent with an abscess wall. The right fallopian tube revealed para-tubal cysts and Walthard cell rests, while the right ovarian cyst was identified as a hemorrhagic corpus luteum. No malignancy was detected in any of the submitted specimens.
Follow-up
Post-operative treatment included intravenous Flagyl (Metronidazole) and Claforan (Cefotaxime), and there were no complications. After six months of follow-up, no significant complication was observed.
Discussion
The development of PID and TOAs has long been considered a rare complication of tubal sterilization. The most frequently isolated pathogens of these abscesses include Escherichia coli and Bacteroides species. Additional identified organisms in these abscesses comprise Peptostreptococcus, Peptococcus, and aerobic Streptococcus species [1]. Although rare, infections involving Staphylococcus species and Burkholderia pseudomallei have also been reported in the literature [6,7]. Among the reviewed cases, six patients developed TOAs following surgical procedures. Among the cases in which microbiological data were reported, Escherichia coli was identified in two patients, Streptococcus pyogenes in another two, and Peptostreptococcus anaerobius in one (Table 1) [1,2,8-12].
|
Author/year |
Age |
Sex |
Pregnancy |
Gynecological history |
Surgical history |
Comorbidities |
Symptoms |
Location |
Mass size (cm)* |
Treatment |
Presence of Foreign Body |
Identified pathogens |
Pathological findings |
Outcome |
|
Sun et al./2024 [9] |
18 |
M |
N/A |
N/A |
Mucocele excision |
None |
Soft and tender nodule |
Lower lip |
1 |
Total excision of the lesion |
Silk suture |
N/A |
Acute and chronic inflammation & multinucleated foreign body giant cells |
Recovery |
|
Linck et al./2023 [16] |
51 |
F |
3 |
Abnormal uterine bleeding |
D&C hysteroscopy & polypectomy |
None |
Heavy menstrual bleeding, fever & abdominal pain |
Right posterior pelvic area |
5.1 |
Antibiotic, Interventional radiology percutaneous drainage, laparotomy, total hysterectomy & bilateral salpingo-oophorectomy |
None |
Escherichia coli |
Acute inflammation & acute serositis |
Recovery |
|
Campbell et al./2021 [2] |
15 |
F |
None |
Unremarkable |
Appendectomy |
None |
Abdominal pain |
Right adnexa |
7.1 |
Laparoscopy, drainage of the right pyosalpinx, removal of the stump appendix & antibiotics |
Stump appendix |
None |
Necrotic material with acute inflammatory debris |
Recovery |
|
Zein et al./2021 [13] |
58 |
M |
N/A |
N/A |
Retinal detachment repair |
HIV infection |
Swollen conjunctivae, bulbar injection, and tearing |
Left eye |
1 |
Corticosteroids, excision of the lesion, & Amniotic membrane transplantation |
Silk suture |
None |
Chronic inflammation |
Recovery |
|
Naredi et al./2021 [15] |
45 |
F |
2 |
Unremarkable |
|
Hypertension & obesity |
Lower abdominal pain |
Left adnexa |
7.6 |
Intravenous antibiotics, drainage, laparotomy & left salpingo-ophrectomy |
N/A |
N/A |
Inflammation |
Recovery |
|
Solt et al./2010 [1] |
24 |
F |
3 |
Menarche at 12 & irregular menstrual cycles |
Colectomy, appendectomy, cesarean deliveries, elective abortion, lami nectomy, breast augmentation & Essure placement |
Mitochondrial neurogastrointestinal encephalopathy, progressive gastrointestinal dysmotility, symmetric polyneuropathy, asymptomatic leukoencephalopathy, asthma, antiphospholipid syndrome, supraventricular tachycardia, renal lithiasis, and bipolar disorder. |
Right lower quadrant pain, nausea, and vomiting |
Right adnexa |
N/A |
Laparoscopy, total abdominal hysterectomy & antibiotics |
Essure microinserts |
Streptococcus pyogenes |
N/A |
Developed acute peritonitis |
|
Weinberger et al./1996 [12] |
34 |
F |
3 |
PID |
Bilateral tubal ligation |
None |
Lower abdominal pain, fever |
Right adnexa |
6.1 |
Antibiotics, adhesiolysis, total abdominal hysterectomy, right salpingo-oophorectomy, & vaginal T-tube drain placement |
Silastic band |
Peptostreptococcus anaerobius |
Acute necrotizing oophoritis |
Recovery |
|
37 |
F |
2 |
Unremarkable |
Bilateral tubal ligation |
None |
bilateral lower quadrant pain, fever, tenderness, vaginal spotting & discharge |
Left adnexa |
4 |
Laparoscopy, laparotomy, bilateral salpingectomies, right oophorectomy, endometrial biopsy, incidental appendectomy & antibiotics |
None |
Streptococcus pyogenes |
Acute suppurative salpingitis, ovarian cortex hemorrhage. Proliferative phase endometrium |
Recovery |
|
|
38 |
F |
2 |
Unremarkable |
Tubal fulguration, kidney transplant |
Systemic lupus erythematosus, immunocompromised |
bilateral lower quadrant pain, fever, tenderness & yellow discharge |
Ovaries |
4.4 |
Laparotomy, bilateral distal salpingectomy & antibiotics. |
None |
Escherichia coli |
Acute suppurative salpingitis & paratubal abscess formation |
Recovery |
|
|
M: Male, F: Female, N/A: Not Available, D&C: Dilation and curettage, HIV: Human immunodeficiency virus, PID: Pelvic inflammatory disease *Only the largest dimension is reported in the table. |
||||||||||||||
Although the exact incidence of upper genital tract infections following surgical sterilization remains unknown, traditional gynecologic literature emphasizes that such occurrences are exceedingly rare. However, other data suggest that the upper genital tract may remain vulnerable to infection even after sterilization. A study found that 6% of hospitalized PID cases involved patients with prior sterilization, with symptoms including systemic toxicity and requiring surgical evaluation in some instances [13].
The postoperative infection in the current patient was caused by the use of silk sutures for tubal ligation. This resulted in the development of a suture abscess, which is a type of foreign body reaction that forms in response to the presence of exogenous suture material introduced during surgery. When this foreign material becomes contaminated with bacterial or fungal organisms, it can lead to the formation of an abscess at the site of the previous surgical procedure [8].
The use of absorbable sutures is preferred for tubal ligations, as they allow the ligated ends to separate naturally over time, thereby reducing the risk of infections and enhancing the effectiveness and permanence of the sterilization [14]. Silk and other multifilament suture materials, on the other hand, permit capillary penetration of bacteria and fluids into the spaces between the filaments, creating an environment that promotes inflammation and increases the risk of both acute and latent infections [15]. This is what is suspected to have happened with the current patient. Post-sterilization infections can manifest within weeks of the procedure or years later. In the present case, the patient developed a TOA three years after undergoing sterilization. Similarly, Weinberger et al. reported three cases of delayed TOA, occurring 8, 15, and 9 years post-sterilization [9]. Suture-related abscesses can present in an even more delayed manner, as demonstrated by Zein et al., who reported a case in which a suture abscess developed 37 years after the original surgical procedure [10].
Efforts to identify predictors for surgical versus antibiotic treatment of TOAs have focused on factors like abscess size, laterality, age, and inflammation severity. Yagur et al. found that bilateral TOAs were more likely to require surgery than unilateral ones, despite no size difference between the two groups. This contrasts with earlier studies, which linked larger abscess size to increased surgical intervention [14]. Among the reviewed cases of TOA, similar to the current patient, surgical intervention was performed in all instances, irrespective of the lesion's laterality or size [1,2,9,11,12]. Currently, the management of TOA typically involves the administration of parenteral broad-spectrum antibiotics. Early diagnosis combined with prompt antibiotic therapy has led to successful medical management in approximately 70–75% of cases. However, the remaining 25–30% of patients require surgical drainage, often utilizing minimally invasive techniques such as laparoscopic drainage or ultrasound-guided transvaginal aspiration and drainage [11]. When managing TOAs, clinicians need to obtain a comprehensive surgical and gynecological history to guide the appropriate therapeutic approach. In cases where a foreign body is suspected or confirmed preoperatively, surgical intervention may offer improved long-term outcomes. A notable limitation of this case report was the absence of microbiological testing. Empirical postoperative treatment was administered based solely on clinical symptoms, which may have limited the ability to definitively identify the underlying pathogen.
Conclusion
Suture-induced TOAs following sterilization may result in considerable morbidity. In these cases, surgical intervention may provide favorable outcomes.
Declarations
Patient consent (participation and publication): Written informed consent was obtained from the patient for publication.
Funding: The present study received no financial support.
Acknowledgements: None to be declared.
Authors' contributions: HMM and NHAA were significant contributors to the conception of the study and the literature search for related studies. SMA, ZMM, OHGH, AGHH, ADS, SOA, LAA, SJJ, and MAA were involved in the literature review, the study's design, and the critical revision of the manuscript, and they participated in data collection. MMA and RMA were involved in the literature review, study design, and manuscript writing. NSS was the radiologist who assessed the case. HMM and MMA confirm the authenticity of all the raw data. All authors approved the final version of the manuscript.
Use of AI: ChatGPT-3.5 was used to assist in language editing and improving the clarity of the manuscript. All content was reviewed and verified by the authors. Authors are fully responsible for the entire content of their manuscript.
Data availability statement: Not applicable.
References
- Solt I, Ioffe Y, Elmore RG, Solnik MJ. Group A streptococcal peritonitis and ruptured tubo-ovarian abscess three years after Essure® insertion: a case report. Journal of Women's Health. 2011;20(5):781-3. doi:10.1089/jwh.2010.2574
- Campbell M, Noor AA, Castaneda M. A case of tubo-ovarian abscess in a 15-year-old female after appendectomy complicated by peritonitis. Cureus. 2021;13(11). doi:10.7759/cureus.20052
- Kreisel K. Prevalence of pelvic inflammatory disease in sexually experienced women of reproductive age—United States, 2013–2014. MMWR. Morbidity and mortality weekly report. 2017;66. doi:10.15585/mmwr.mm6603a3
- Kakamad FH, Abdalla BA, Abdullah HO, Sami S. Omar, Shvan H. Mohammed, Sasan M. Ahmed, et al. Lists of predatory journals and publishers: a review for future refinement. Eur Sci Ed. 2024;50:e118119. doi:10.3897/ese.2024.e118119
- Prasad S, Nassar M, Azzam AY, García-Muro-San José F, Jamee M, Sliman RK, et al. CaReL Guidelines: A Consensus-Based Guideline on Case Reports and Literature Review (CaReL). Barw Med J. 2024;2(3):13-19 doi:10.58742/bmj.v2i2.89
- Pickering KD, Smith DO. Tubo-ovarian abscess after tubal ligation. The West Indian Medical Journal. 1998;47(3):113-4. doi:N/A
- Nernsai P, Sophonsritsuk A, Lertvikool S, Jinawath A, Chitasombat MN. A case report of Tubo-ovarian abscess caused by Burkholderia pseudomallei. BMC infectious diseases. 2018;18:1-4. doi:10.1186/s12879-018-2986-z
- Sun A, Lee YP, Jin YT, Chiang CP. Silk suture granuloma with abscess in the lower lip. Journal of Dental Sciences. 2024;19(4):2464. doi: 10.1016/j.jds.2024.06.006
- WEINBERGER MW, O'CONNELL BJ, JULIAN TM. Tuboovarian abscess after tubal sterilization: A report of three cases and literature review. Journal of gynecologic surgery. 1996;12(4):267-70. doi:10.1089/gyn.1996.12.267
- Zein M, Theotoka D, Wall S, Galor A, Cabot F, Patel U et al. Silk suture granuloma 37 years after scleral buckle surgery: a case report. Cornea. 2021;40(10):1357-9. doi:10.1097/ico.0000000000002637
- Naredi N, Prajapati VK, Mhaske N, Sahay N. Sequential radiological and surgical management of tubo-ovarian abscess: a success story. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2021;10(6):2542. doi:10.18203/2320-1770.ijrcog20212214
- Linck JH, Torres WI, Dayal ST, Linck J. Post-hysteroscopy Ruptured Tubo-Ovarian Abscess With Atypical Bacteremia: A Case Report. Cureus. 2023;15(9). doi:10.7759/cureus.45618
- Green MM, Vicario SJ, Sanfilippo JS, Lochhead SA. Acute pelvic inflammatory disease after surgical sterilization. Annals of emergency medicine. 1991 Apr 1;20(4):344-7. doi:10.1016/S0196-0644(05)81651-8
- Peterson HB. Sterilization. Obstetrics & Gynecology. 2008;111(1):189-203. doi:10.1097/01.aog.0000298621.98372.62
- Calkins CM, St. Peter SD, Balcom A, Murphy PJ. Late abscess formation following indirect hernia repair utilizing silk suture. Pediatric surgery international. 2007;23:349-52. doi:10.1007/s00383-007-1894-x
- Yagur Y, Weitzner O, Shams R, Man-El G, Kadan Y, Daykan Y et al. Bilateral or unilateral tubo-ovarian abscess: exploring its clinical significance. BMC Women's Health. 2023;23(1):678. doi:10.1186/s12905-023-02826-x

This work is licensed under a Creative Commons Attribution 4.0 International License.

