Presentation and Management of Cervical Thoracic Duct Cyst: A Systematic Review of the Literature
Abstract
Introduction
Thoracic duct cysts are an uncommon phenomenon, especially within the cervical region. Due to its limited reported cases, very little is known about its etiology, presentation, and management. This systematic review is conducted to shed light on the ways the cyst presents and the outcomes of different treatment regimens.
Methods
The EMBASE, CINAHL, PubMed/MEDLINE, Cochrane Library, and Web of Science databases were thoroughly screened to identify any studies published in English up to March 24th, 2024.
Results
The average age of the patients was 47.8 years, with 9 (56.3%) females in the study population. The mean size of the cysts was 5.99 cm, and the most common symptom was pain, present in 5 (31.3%) patients. The most common management approach chosen for 6 (37.5%) patients was simple follow-up and observation, followed by surgical excision in 5 (31.3%) patients.
Conclusion
Patients with thoracic duct cervical cysts may be asymptomatic or present with pain. Both surgical excision and conservative management may yield satisfactory outcomes.
Introduction
The thoracic duct runs 38 to 45 centimeters from the cysterna chyli at L2 vertebral level to the lower cervical spine [1]. The duct is 2 to 5 millimeters wide, and it carries lymph ingested with fat from the vascular bed of the gastrointestinal system and drains into the central veins of the neck [1,2]. Very rarely, a cyst develops from the thoracic duct, also called a lymphocele of the thoracic duct [3]. The pathology is very uncommon, even more so in the cervical segment, since among the limited reported cases, the majority have been documented as either a thoracic or an abdominal thoracic duct cyst [4]. Although not established, theories suggest that congenital thoracic duct weakness and inflammation-mediated degeneration of the duct can predispose to cyst formation [5]. Due to the limited number of cases reported, no gold standard treatment has been established for cervical thoracic duct cysts; however, both surgical and conservative management have been proposed. To our knowledge, this is the first review in the literature about cervical thoracic duct cysts. This study aims to contribute to the literature by summarizing presentations, management, and outcomes of reported cases of cervical thoracic duct cysts.
Methods
Study design
The guideline followed in this systematic review was that of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines. Any study with a reported case of a cervical thoracic cyst was included, provided that necessary information was given on the patient and the mass.
Data sources and search strategy
EMBASE, CINAHL, PubMed/MEDLINE, Cochrane Library, and Web of Science databases were all screened using the following ("Thoracic duct" AND Cyst OR Cysts AND Neck OR Cervical) keywords.
Eligibility criteria
Any study with a reported case of thoracic duct cyst found within the cervical region and published in English was deemed eligible. Information on the patient, as well as the characteristics of the cyst, was required. To avoid bias, any study published in predatory journals, identified using Kscien’s list, was excluded from this systematic review [6].
Study selection process
The titles and abstracts of the enrolled studies were screened by two different researchers, attempting to identify papers based on the study's eligibility criteria. A third researcher was recruited to resolve any disagreements that might arise between the initial two researchers.
Data items
Data was collected on mean age, sex, type of study, country of study, presentation, type of symptoms, location of the cyst, size of the cyst, management, and outcome of each management.
Statistical analysis
Microsoft Excel Workbook sheet was used to record the extracted data. The Statistical Package for Social Sciences (SPSS) 26.0 software was used in further quantitative analysis. The data is presented as frequencies and percentages.
Results
Study selection
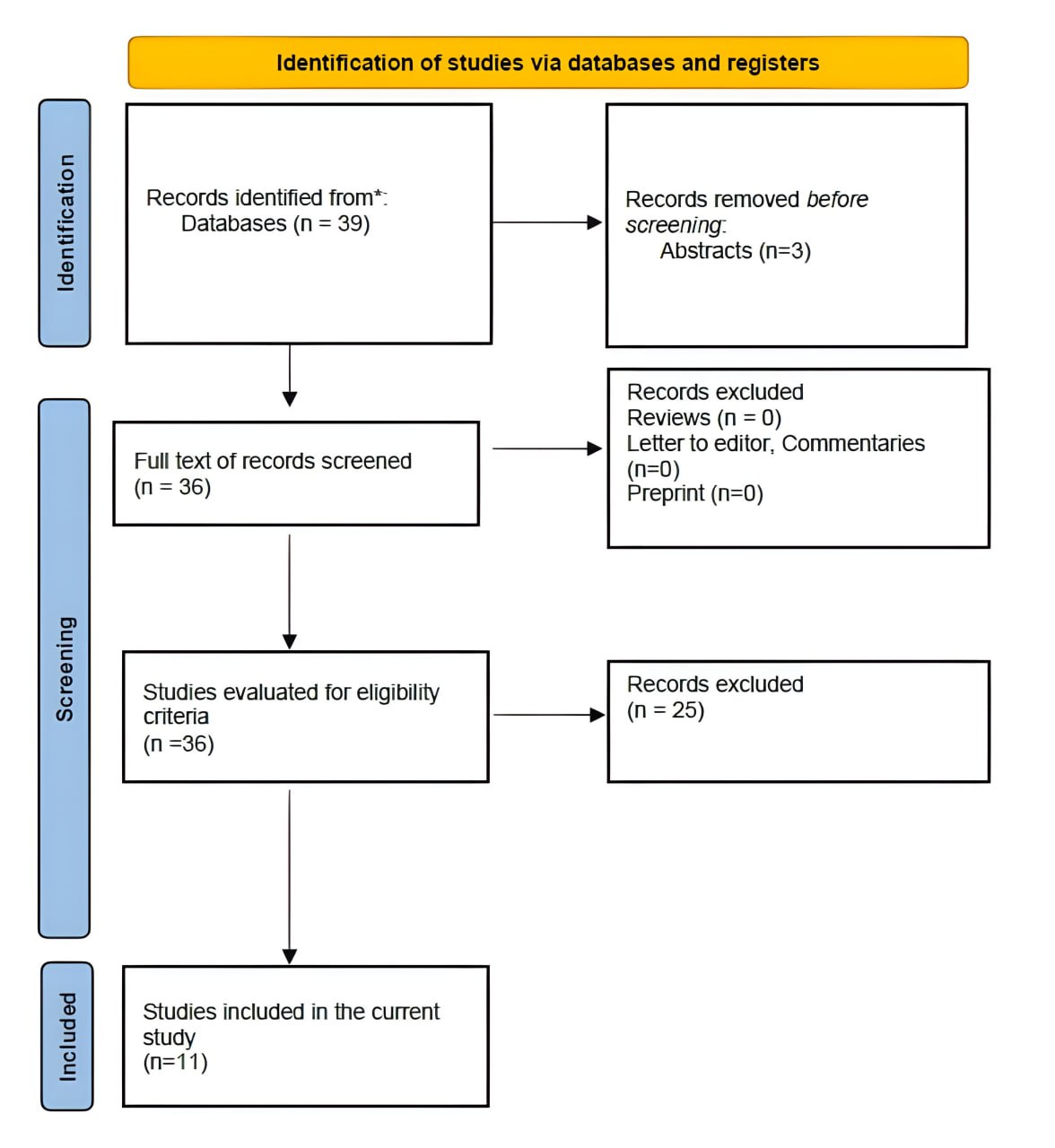
The systematic search first brought 39 papers. Out of the initial 39, three only-abstract studies were excluded without further screening. The remaining 36 papers had their titles and abstracts screened, which resulted in 25 papers being removed due to irrelevancy. No paper was excluded due to wrong designs. The remaining 11 [4,7-16] studies were checked for wrong outcomes and predatory publishing; however, none were found. This left 11 papers at last to be included in this systematic review. The PRISMA flow chart highlights more details (Figure 1).
Characteristics of the included studies
Among the 11 included studies, 10 (91%) were case reports, with only one (9%) study being a case series. The United States, with four (36.3%), and France, with two (18.2%) studies, contributed the most, followed by Greece, China, Finland, Norway, and Canada, each with one study.
Main findings
A total of 16 patients were included in this systematic review. The average age of the patients was 47.8 ± 17.8 years. There were nine (56.3%) females compared to six (37.5%) males, leaving one (6.2%) patient unspecified. Half of the patients were symptomatic, and pain was the sole symptom in four (25%) patients. Details on the baseline observation and follow-up of the cyst were done for six (37.5%) patients, followed by surgical excision in five (31.4%) patients, a low-fat diet for two (12.5%) patients, aspiration performed in one (6.2%) patient, and lastly, one (6.2%) patient who underwent both surgical excision and had also received a low-fat diet modification regimen. All (100%) patients had their mass in the left supraclavicular region. The outcome of 12 (75%) patients was to be discharged without complications, whereas one (6.2%) patient was observed to have a persistent mass, and three (18.8%) patients did not have their outcome mentioned (Tables 2 and 3).
|
Author/ year of publication |
Type of Study |
Country of study |
Age (years) |
Sex |
Presentation |
Type of symptoms |
|
Brauchle et al. 2003 [4] |
Case report |
United States |
41 |
Male |
Asymptomatic |
N/A |
|
Mattila et al. 1999 [7] |
Case report |
Finland |
49 |
Female |
Asymptomatic |
N/A |
|
Metaxas et al. 2021 [8] |
Case report |
Greece |
42 |
Male |
Symptomatic |
Pain |
|
Wang et al. 2009 [9] |
Case report |
China |
28 |
Female |
Asymptomatic |
N/A |
|
Veziant et al. 2015 [10] |
Case report |
France |
49 |
Female |
Symptomatic |
Pain and Dyspnea |
|
Planchette et al. 2021 [11] |
Case series |
France |
50 |
Male |
Asymptomatic |
N/A |
|
74 |
Female |
Asymptomatic |
N/A |
|||
|
45 |
Female |
Symptomatic |
Pain |
|||
|
65 |
Female |
Asymptomatic |
N/A |
|||
|
64 |
Female |
Symptomatic |
Pain |
|||
|
62 |
Female |
Symptomatic |
Pain |
|||
|
Bhalla et al. 2017 [12] |
Case report |
United States |
0.67 |
Male |
Symptomatic |
Dyspnea |
|
Steinberg 1964 [13] |
Case report |
United States |
56 |
Female |
Symptomatic |
Migraine headaches |
|
Steinberg & Watson 1966 [14] |
Case report |
United States |
28 |
N/A |
Symptomatic |
Soreness |
|
Kolbenstvedt et al. 1986 [15] |
Case report |
Norway |
55 |
Male |
Asymptomatic |
N/A |
|
Wax et al. 1992 [16] |
Case report |
Canada |
56 |
Male |
Asymptomatic |
N/A |
|
Author/ year of publication |
Age (years) |
Location of cyst |
Size of cyst |
Management |
Outcome |
|
Brauchle et al. 2003 [4] |
41 |
Left supraclavicular |
4 cm |
Aspiration |
Patient was discharged |
|
Mattila et al. 1999 [7] |
49 |
Left supraclavicular |
3.8 cm |
Surgical Excision |
Patient was discharged |
|
Metaxas et al. 2021 [8] |
42 |
Left Neck |
N/A |
Surgical Excision |
Patient was discharged |
|
Wang et al. 2009 [9] |
28 |
Left supraclavicular |
10 cm |
Surgical Excision |
Patient was discharged |
|
Veziant et al. 2015 [10] |
49 |
Left supraclavicular |
3 cm |
Surgical Excision |
Patient was discharged |
|
Planchette et al. 2021 [11] |
50 |
Left supraclavicular |
N/A |
Follow up |
Patient was discharged |
|
74 |
Left supraclavicular |
N/A |
Follow up |
Patient was discharged |
|
|
45 |
Left supraclavicular |
N/A |
Follow up |
Patient was discharged |
|
|
65 |
Left supraclavicular |
N/A |
Follow up |
N/A |
|
|
64 |
Left supraclavicular |
N/A |
Low fat diet |
Patient was discharged |
|
|
62 |
Left supraclavicular |
N/A |
Low fat diet |
Patient was discharged |
|
|
Bhalla et al. 2017 [12] |
0.67 |
Left supraclavicular |
13.1 cm |
Surgical drainage and low fat diet |
Patient was discharged |
|
Steinberg 1964 [13] |
56 |
Left supraclavicular |
3 cm |
N/A |
N/A |
|
Steinberg & Watson 1966 [14] |
28 |
Left supraclavicular |
3 cm |
Follow up |
N/A |
|
Kolbenstvedt et al. 1986 [15] |
55 |
Left supraclavicular |
3 cm |
Follow up |
Mass persistence |
|
Wax et al. 1992 [16] |
56 |
Left supraclavicular |
10 cm |
Surgical Excision |
Patient was discharged |
|
Variables |
Frequency/percentage |
|
Age (mean ± SD) |
47.8 ± 17.8 years |
|
Sex Male Female N/A |
Number of patients (16) 6 (37.5%) 9 (56.3%) 1 (6.2%) |
|
Country of study United States France Greece China Finland Norway Canada |
Number of studies (11) 4 (36.3%) 2 (18.2%) 1 (9.1%) 1 (9.1%) 1 (9.1%) 1 (9.1%) 1 (9.1%) |
|
Type of Study Case report Case series |
Number of studies (11) 10 (90.1%) 1 (9.9%) |
|
Presentation Symptomatic Asymptomatic |
Number of patients (16) 8 (50%) 8 (50%) |
|
Type of symptoms Pain Pain and dyspnea Dyspnea Migraine Soreness N/A |
Number of patients (16) 4 (25%) 1 (6.2%) 1 (6.2%) 1 (6.2%) 1 (6.2%) 8 (50%) |
|
Size of cyst (mean ± SD) |
5.99 ± 3.99 cm |
|
Management Aspiration Surgical Excision Follow up Low-fat diets Surgical excision & low-fat diet N/A |
Number of patients (16) 1 (6.2%) 5 (31.4%) 6 (37.5%) 2 (12.5%) 1 (6.2%) 1 (6.2%) |
|
Outcome Patient was discharged Mass persisted N/A |
Number of patients (16) 12 (75%) 1 (6.2%) 3 (18.8%) |
|
* N/A: Not applicable |
|
Discussion
Apart from the right side of the upper extremity, the right side of the thorax, and the right side of the neck, the thoracic duct drains the lymphatics of the rest of the body [1]. An uncommon phenomenon related to the duct is a thoracic duct cyst, also called a lymphocele of the thoracic duct [3]. Theoretically, the cyst can arise throughout the length of the entire duct; however, it usually arises within either the thorax or the abdomen. A thoracic lymphocele of the cervical region is the rarest form [4]. A cervical thoracic duct cyst will present as a lateral neck mass arising from the supraclavicular fossa. In this systematic review, all 16 patients presented with a mass, either painful or not, within the left supraclavicular fossa. Bhalla et al. reported the youngest patient recorded in the literature with a thoracic duct lymphocele presenting in an 8-month-old boy [12]. According to Abelarado et al., the cyst tends to occur more frequently in females, and the average age among the patients presenting with the cyst is 49.8 years [15]. This is in accordance with the current study’s findings, as the average age was 47.8 ± 17.8 years, and the majority were females. No single factor has been identified as a cause of this pathology; however, inflammation-mediated degeneration of the duct wall and congenital weakness have been suggested, as well as any possible traumas [3].
As previously mentioned, since the duct drains the left side of the neck, the cyst will present as a left-sided supraclavicular mass. Most patients with a thoracic duct lymphocele are asymptomatic [5]. Half of the patients in this systematic review were symptomatic, and the other half had no complaints. Symptoms are generally due to the compressive effect of the mass on adjacent structures and can include pain, dysphagia,
cyanosis, and even respiratory distress [7]. In this study, four (25%) patients presented with pain alone, making it the most common symptom. Others, such as migraine headaches, dyspnea, and soreness, were also reported, with one patient suffering from both pain and dyspnea. Lymphoscintigraphy used to be considered the gold standard for diagnosis; however, with the advent of new high-resolution imaging techniques, this tool has become less popular [17]. Confirmation of the diagnosis is usually conducted during surgery, as histological analysis of the specimen can be beneficial. One way this is done is by staining the endothelial cells lining the thoracic duct to verify that the cyst is, in fact, a thoracic duct cyst [4,18]. According to Mattila et al., another way to diagnose a thoracic duct cyst is via puncture and subsequence analysis. Following aspiration, the aspirate will manifest as a milky fluid showing excess triglyceride in laboratory investigations and lymphocytes, neutrophils, and macrophages, among others [7].
Regarding management, no single gold standard has been established. This is attributed to the low number of cases that have been recorded. As previously mentioned, aspiration, although usually performed for diagnosis purposes, can be sufficient to deal with the mass. In this review, only one of the patients had aspiration alone. Surgical excision of the thoracic duct cyst is another common way to manage the mass [7]. This was performed for five (31.4%) patients in this review. Interestingly, in some instances, and especially after deeming the mass nonneoplastic, patients are followed up and observed after they either refuse surgery or the physician doesn’t consider it necessary. This has been highlighted in six (37.5%) patients within this study’s population. Furthermore, patients were managed through diet modification and, more specifically, transitioning to a low-fat diet. This yielded a satisfactory outcome in the two patients who only received diet modification and in the one patient who underwent surgical excision followed by a transition to a low-fat diet. All different management methods yielded satisfactory outcomes, with patients discharged without complications in three-quarters of the cases. This was apart from one patient whose mass persisted since they underwent no management and were observed.
Conclusion
Patients with thoracic duct cervical cysts may be asymptomatic or present with pain. Both surgical excision and conservative management may yield satisfactory outcomes.
Declarations
Conflicts of interest: The authors have no conflicts of interest to disclose.
Ethical approval: Not applicable, as systematic reviews do not require ethical approval.
Patient consent (participation and publication): Not applicable.
Funding: The present study received no financial support.
Acknowledgements: None to be declared.
Authors' contributions: FHK and BAA were significant contributors to the conception of the study and the literature search for related studies. DSH and ASA involved in the literature review, study design, and manuscript writing. AJQ, RJR, MLF, STSA, ASM, and HOB were involved in the literature review, the study's design, the critical revision of the manuscript, and data collection. FHK and DSH confirm the authenticity of all the raw data. All authors approved the final version of the manuscript.
Use of AI: ChatGPT-3.5 was used to assist in language editing and improving the clarity of the manuscript. All content was reviewed and verified by the authors. Authors are fully responsible for the entire content of their manuscript.
Data availability statement: Not applicable.
References
- Ilahi, Maira, et al. “Anatomy, Thorax, Thoracic Duct.” PubMed, StatPearls Publishing, 2022, pubmed.ncbi.nlm.nih.gov/30020599/. 2023. doi:N/A
- Phang K, Bowman M, Phillips A, Windsor J. Review of thoracic duct anatomical variations and clinical implications. Clinical anatomy. 2014 ;27(4):637-44. doi:10.1002/ca.22337
- Offiah CE, Twigg S. Lymphocoele of the thoracic duct: a cause of left supraclavicular fossa. The British journal of radiology. 2011 ;84(998):e27-30. doi:10.1259/bjr/28200085
- Brauchle RW, Risin SA, Ghorbani RP, Pereira KD. Cervical thoracic duct cysts: a case report and review of the literature. Archives of Otolaryngology–Head & Neck Surgery. 2003;129(5):581-3. doi:10.1001/archotol.129.5.581
- Farouk A, Weerakkody Y, Bell D, et al. Lymphocele of the thoracic duct. Reference article, Radiopaedia.org. doi:10.53347/rID-56163
- Muhialdeen AS, Ahmed JO, Baba HO, Abdullah IY, Hassan HA, Najar KA, Mikael TM, Mustafa MQ, Mohammed DA, Omer DA, Bapir R. Kscien’s list; a new strategy to discourage predatory journals and publishers (second version). Barw Medical Journal. 2023. doi:10.58742/bmj.v1i1.14
- Mattila PS, Tarkkanen J, Mattila S. Thoracic duct cyst: a case report and review of 29 cases. Annals of Otology, Rhinology & Laryngology. 1999 ;108(5):505-8. doi:10.1177/000348949910800516
- Metaxas EK, Noussi G. THORACIC DUCT CYST IN THE LE REPORT AND LITE. doi:10.24941/ijcr.41442.06.2021
- Wang YA, Zhang ZY, Zheng JW, Ye WM, Wang LZ, Zhu HG. Spontaneous thoracic duct cyst presenting as a left supraclavicular mass–report of a case and review of literature. Phlebology. 2009 ;24(2):82-4. doi:10.1258/phleb.2008.008056
- Veziant J, Sakka L, Galvaing G, Tardy MM, Cassagnes L, Filaire M. Lymphovenous anastomosis for recurrent swelling syndrome and chylous effusion due to cervical thoracic duct cyst. Journal of Vascular Surgery. 2015 ;62(4):1068-70. doi:10.1016/j.jvs.2014.02.060
- Planchette J, Jaccard C, Nigron A, Chadeyras JB, Le Guenno G, Castagne B, et al. Recurrent thoracic duct cyst of the left supraclavicular fossa: A retrospective study of 6 observational case series and literature review. Medicine. 2021 ;100(50):e28213. doi:10.1097/md.0000000000028213
- Bhalla V, Schrepfer T, McCann A, Nicklaus P, Reading B. Spontaneous retropharyngeal and mediastinal thoracic duct cyst in an infant with respiratory distress. International journal of pediatric otorhinolaryngology. 2018 ;105:33-5. doi:10.1016/j.ijporl.2017.11.021
- Steinberg I. Roentgen diagnosis of persistent jugular lymph sac. Radiology. 1964 ;82(6):1022-3. doi:10.1148/82.6.1022
- Steinberg I, Watson RC. Lymphangiographic and angiographic diagnosis of persistent jugular lymph sac: report of a case. New England Journal of Medicine. 1966 ;275(26):1471-4. doi:10.1056/nejm196612292752604
- Kolbenstvedt A, Aanesen J. Cystic dilatation of the thoracic duct presenting as a supraclavicular mass. The British Journal of Radiology. 1986 ;59(708):1228-9. doi:10.1259/0007-1285-59-708-1228
- Wax MK, Treloar ME. Thoracic duct cyst: an unusual supraclavicular mass. Head & neck. 1992 ;14(6):502-5. doi:10.1002/hed.2880140615
- Dortch JD, Eck DL, Hakaim AG, Casler JD. Management of cervical thoracic duct cyst with cyst-venous anastomosis. International Journal of Surgery Case Reports. 2014 ;5(12):1028-30. doi:10.1016/j.ijscr.2014.10.012
- Chen F, Bando T, Hanaoka N, Terada Y, Ike O, Wada H, et al. Mediastinal thoracic duct cyst. Chest. 1999 ;115(2):584-5. doi:10.1378/chest.115.2.584

This work is licensed under a Creative Commons Attribution 4.0 International License.

