Perceptions of Telemedicine and Rural Healthcare Access in a Developing Country: A Case Study of Bayelsa State, Nigeria
Abstract
Introduction
Telemedicine is the remote delivery of healthcare services using information and communication technologies and has gained global recognition as a solution to address healthcare disparities. This study explores the perceptions of telemedicine and its potential to improve rural healthcare access in a developing country through the insights of undergraduate Medical Laboratory Science students.
Methods
A descriptive cross-sectional study was conducted among 42 fourth-year students of the Medical Laboratory Science program. Respondents completed a structured questionnaire that assessed their awareness, familiarity, perceived benefits and barriers to telemedicine, and their views on its applicability in rural Bayelsa.
Results
The findings indicated that while the majority of respondents (60.5%) were aware of telemedicine, their understanding of specific types, such as asynchronous and synchronous telehealth, was limited. The main perceived benefits were improved healthcare access (48.8%) and reduced costs (18.6%). Acceptance levels varied, with 47.6% endorsing telemedicine, while others remained uncertain or sceptical.
Conclusion
The study reveals enthusiasm and knowledge gaps among future healthcare professionals regarding telemedicine. It highlights the need for targeted education, digital literacy, and infrastructure investment to enable telemedicine in rural Nigerian communities.
Introduction
Telemedicine, the remote delivery of healthcare services using information and communication technologies (ICTs), has emerged as a transformative strategy for improving healthcare access, particularly in rural and underserved regions [1]. Overcoming geographical and logistical barriers enables timely consultations, diagnostics, and follow-up care without requiring long-distance travel.
In many developing countries, telemedicine has become an increasingly important solution for bridging healthcare gaps caused by workforce shortages, underdeveloped infrastructure, and rural-urban healthcare disparities. Low- and middle-income countries (LMICs) in Africa and Asia have seen gradual adoption of digital health technologies, including mobile health (mHealth) platforms and virtual consultations, especially during and after the COVID-19 pandemic [2]. While countries such as Rwanda, Ghana, and India have launched national digital health strategies, challenges like unreliable internet, funding limitations, and limited technical literacy continue to affect large-scale implementation [3]. Within this global context, Nigeria shares many of these challenges but also presents unique opportunities for leveraging telemedicine in improving rural healthcare access.
In Nigeria, where disparities in healthcare access are especially pronounced in rural areas, telemedicine holds considerable promise. Previous studies have demonstrated its benefits like reduced patient travel time and improved early diagnosis rates. Other studies found that telemedicine enhanced antenatal care coverage in rural communities in Enugu. These findings emphasise the potential of telemedicine in addressing healthcare disparities in diverse Nigerian settings [4,5].
However, the country's healthcare infrastructure and human resources remain critically inadequate, with a disproportionate concentration in urban areas [6]. Rural residents, who make up over 40% of the Nigerian population, face poor access to quality and affordable healthcare. Physical distance, limited transportation, and high travel costs often delay or prevent illness treatment, especially in geographically isolated areas [7]. These challenges have resulted in adverse health outcomes, including higher rates of infectious diseases and maternal and child mortality in rural communities. Telemedicine offers an opportunity to address these inequities by connecting healthcare providers with rural populations through virtual consultations and mobile health technologies [8]. Mobile platforms, in particular, facilitate affordable and convenient care delivery in settings lacking comprehensive health infrastructure.
While telemedicine has demonstrated significant potential in rural regions across Africa, successful implementation remains context-dependent, requiring adaptation to local infrastructure and socio-cultural realities [9]. Despite its benefits, the widespread adoption of telemedicine in Nigeria remains limited due to persistent challenges such as unreliable internet connectivity, the high cost of digital tools, and low levels of digital literacy among both healthcare workers and patients [10]. These challenges are even more pronounced in Bayelsa State, a region in Nigeria's Niger Delta known for its swampy terrain, scattered riverine communities, and poor road infrastructure [11,12]. Given these constraints, Bayelsa stands out as a strong candidate for targeted telemedicine interventions. However, there is a notable gap in data regarding local perceptions and readiness, particularly in these uniquely challenging settings.
In this context, telemedicine may enhance healthcare delivery by mitigating travel-related barriers through remote diagnostics, video consultations, and mobile health applications. However, developing effective implementation strategies requires an understanding of local awareness, perceptions, and barriers to the use of telemedicine.
In Nigeria, understanding local perceptions is critical to designing effective, context-specific telemedicine interventions. This study focuses on Bayelsa State, located in the country's Niger Delta region. It explores the perceived impact of telemedicine on healthcare access through the insights of 400-level Medical Laboratory Science students at Niger Delta University. These students represent a well-educated segment of the rural population, many of whom live in or maintain close ties with underserved communities. Their clinical training equips them with a foundational understanding of healthcare systems and digital innovations, such as telemedicine, allowing them to assess its applicability critically.
Furthermore, as future healthcare professionals, their perspectives offer valuable insight into both community needs and the likelihood of professional adoption of telemedicine. Their dual role as rural community members and emerging practitioners provides a unique vantage point for evaluating the feasibility, acceptance, and scalability of telemedicine. The findings aim to inform evidence-based policy and program strategies that could enhance healthcare access in geographically disadvantaged regions like Bayelsa State.
Methods
Study area
This study was conducted among 400-level students in the Department of Medical Laboratory Science at Niger Delta University, located in Bayelsa State, Nigeria. The university is situated in a region with significant rural and riverine communities, making it relevant for healthcare access and telemedicine research.
Study design
A descriptive cross-sectional study assessed perceptions of telemedicine and its potential impact on healthcare access in rural communities.
Population and sample size
The target population comprised all 400-level students enrolled in the Department of Medical Laboratory Science at Niger Delta University. Participants were selected based on their willingness and availability to respond to the questionnaire. This population was chosen because it represents a group of emerging healthcare professionals who are academically exposed to modern healthcare systems and likely to engage with digital health solutions in their future careers. As senior students in a clinical field, their perspectives offer valuable insights into the readiness and acceptance of telemedicine among the next generation of practitioners. Furthermore, their residence in Bayelsa State ensures contextual relevance, as they can relate professionally and personally to the healthcare access challenges faced in the region.
Data collection instruments
The primary instrument for data collection was a structured questionnaire developed using Google Forms. The questionnaire consisted of both closed-ended and open-ended questions designed to assess respondents' demographics, awareness of telemedicine, perceived benefits, challenges, and preferred access modes.
Data collection procedure
The Google Form link containing the questionnaire was distributed electronically via WhatsApp to prospective participants. Respondents accessed and completed the form using their electronic devices.
Statistical analysis
Descriptive statistics were used to summarise the data. The results are presented in tables and charts to illustrate key findings clearly.
Results
The majority of respondents were aged 21–25 years, indicating a predominance of young adults (Table 1). Most respondents were female (64.3%), while males comprised 35.7%.
|
Age Group (Years) |
Number of Respondents |
Percentage (%) |
|
16–20 |
4 |
9.52% |
|
21–25 |
28 |
66.67% |
|
26–30 |
5 |
11.90% |
|
31–35 |
5 |
11.90% |
|
Total |
42 |
100% |
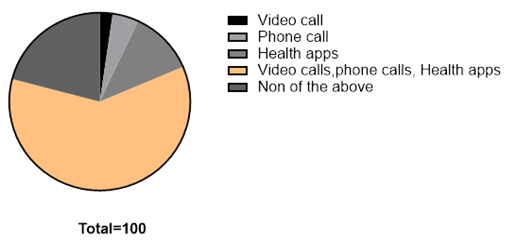
The most frequently reported challenge to accessing healthcare was the high cost of healthcare services, cited by 50% of respondents. Other notable barriers included a shortage of medical personnel (21.4%) and long travel distances to healthcare facilities (14.3%). A smaller proportion of respondents either did not know where to access services (2.4%) or identified other issues, such as long wait times or inadequate infrastructure (11.9%) (Table 2). When asked what came to mind when thinking of telemedicine, 60.5% selected the combination of video calls, phone calls, and health applications. Smaller groups identified health apps alone (11.6%), phone calls (4.7%), or video calls (2.3%), while 20.9% indicated they were unfamiliar with the concept (Figure 1).
|
Challenge |
Number of Respondents |
Percentage (%) |
|
Too far |
6 |
14.29% |
|
Too expensive |
21 |
50.00% |
|
No Medical personnel |
9 |
21.43% |
|
Do not know where to go |
1 |
2.38% |
|
Others |
5 |
11.91% |
|
Total |
42 |
100% |
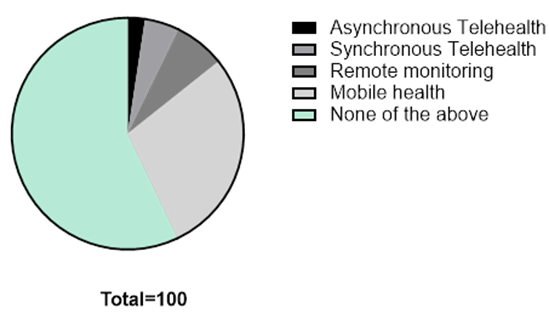
In terms of familiarity with specific types of telemedicine, 58.1% of respondents reported no awareness. Among the remaining respondents, 27.9% were familiar with mobile health (mHealth), 7% with remote monitoring, 4.7% with synchronous telehealth, and 2.3% with asynchronous telehealth (Figure 2).
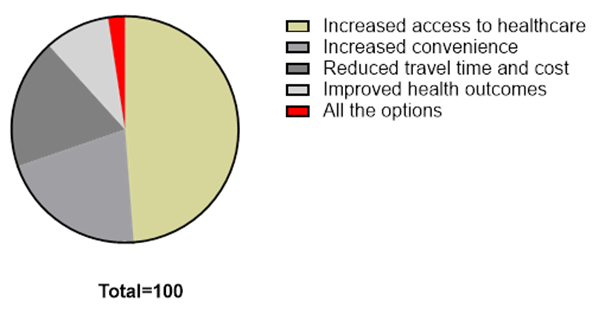
Regarding the perceived benefits of telemedicine, 48.8% of respondents identified increased healthcare access as an important advantage. Other selected benefits included convenience (20.9%), reduced travel time and cost (18.6%), and improved health outcomes (9.3%). Only 2.4% selected "all the options" (Figure 3).
Discussion
Nigeria's healthcare system has consistently struggled to meet the demands of its rapidly growing population, which has surpassed 200 million [13,14].
Findings revealed that most respondents recognised telemedicine as involving video calls, phone calls, and health applications, indicating a broad level of general awareness. However, knowledge of specific categories such as asynchronous and synchronous telehealth was limited. This gap between general familiarity and specific understanding suggests the need for targeted education and capacity-building to support effective adoption of telemedicine services in rural communities.
The distribution of respondents across urban and rural backgrounds further underscored the relevance of telemedicine in both settings. However, its utility is particularly critical in rural areas where persistent barriers, such as travel distance, lack of transport, and shortage of healthcare professionals, continue to hinder timely access to care [15]. These issues are especially prevalent in geographically complex regions like Bayelsa State.
Healthcare-seeking behaviour among respondents also reflected patterns consistent with young adult populations, with many reporting infrequent visits to health facilities. This may be due to a combination of factors, including cost, convenience, and perceived need. Telemedicine presents an opportunity to address this behavioural trend by offering more accessible, flexible, and digitally enabled healthcare services suitable for this demographic.
Respondents identified high healthcare costs, shortage of medical personnel, and travel distance as the main barriers to accessing care. These findings align with previous research highlighting cost and provider shortages as critical obstacles to healthcare access in Nigeria [13-16]. In Bayelsa, the challenges are compounded by infrastructural limitations and rugged terrain. Telemedicine can mitigate these access issues by facilitating remote consultations, reducing the need for travel, and expanding the reach of healthcare professionals [17].
Although nearly half of the respondents expressed positive attitudes toward telemedicine, a significant portion remained either unsure or not in support. This suggests that awareness alone does not guarantee acceptance. Other factors, such as trust in virtual consultations, digital literacy levels, and user experience, may likely influence attitudes toward adoption. Similar findings in the literature indicate that successful implementation requires more than infrastructure; it must also involve building community trust and providing user-friendly, culturally appropriate solutions [18].
Supporting evidence confirms that a deeper understanding of telemedicine correlates with greater satisfaction and willingness to use digital health services [19]. The challenges reported in this study are consistent with known access barriers, reinforcing telemedicine's potential to address the structural limitations affecting rural healthcare delivery [16,20]. Prior studies have shown that telemedicine can reduce travel time, enable early diagnoses, and increase the efficiency of healthcare systems [15,19]. These benefits are particularly valuable in low-resource settings.
Interestingly, while much of the literature highlights internet connectivity and the cost of digital tools as primary barriers, respondents in this study placed more emphasis on the affordability and availability of healthcare services themselves [9]. This suggests that for students and communities in Bayelsa, immediate access to care is a more pressing concern than the infrastructure required to support digital health. In regions where core health services are still lacking, addressing foundational healthcare needs may take precedence over technological investments.
As with all self-reported data, there is a potential for response bias influenced by individual beliefs or differing levels of exposure to digital health tools.
Conclusion
The findings of this study broadly support existing literature affirming telemedicine's potential to improve healthcare access in Nigeria. The study underscores the need for context-specific, targeted strategies in implementing telemedicine, especially approaches that address affordability, community trust, and digital literacy. Future studies should examine broader stakeholder readiness, infrastructure challenges, and user training needs to guide effective policy and implementation.
Declarations
Conflicts of interest: The authors have no conflicts of interest to disclose.
Ethical approval: This study was granted by the Research Ethics Committee of Niger Delta University.
Patient consent (participation and publication): Was obtained from all participants prior to completing the questionnaire, and participants were assured of confidentiality and anonymity.
Funding: The present study received no financial support.
Acknowledgements: None to be declared.
Authors' contributions: CFO conceptualised the idea and collected the data, while ELL wrote the manuscript and analysed the data. All authors read and approved the manuscript.
Use of AI: Grammarly was used to assist in language editing and improving clarity. All content was reviewed and verified by the authors.
Data availability statement: Not applicable.
References
- Key World Health Organization. Telemedicine: Opportunities and developments in Member States: Report on the second global survey on eHealth 2009. Geneva: WHO; 2010. https://iris.who.int/handle/10665/44497
- Iyengar K, Jain VK, Vaishya R. Pitfalls in telemedicine consultations in the era of COVID-19 and how to avoid them. Diabetes Metab Syndr. 2020;14(5):797–9. doi:10.1016/j.dsx.2020.06.007
- World Health Organization. Global strategy on digital health 2020–2025. Geneva: WHO; 2021 [cited 2025 Sep 2]. Available from: https://www.who.int/publications/i/item/9789240020924
- Ukpe E. Transforming healthcare: Telemedicine's role and impact in Nigeria. J Humanit Soc Sci. 2025;30(2):20–6.
- Eze PN, Okafor JC, Nwachukwu LA. Enhancing maternal health through telemedicine in rural Enugu communities. Afr J Reprod Health. 2024;18(1):33–45.
- Pezzuto I. Making healthcare systems more efficient and sustainable in emerging and developing economies through disruptive innovation: The case of Nigeria. J Manag Sustain. 2019;9(1):1–12. https://doi.org/10.5539./jms.v9n2p1
- Ikumapayi OM, Kayode JF, Afolalu SA, Bodunde OP. Telehealth and telemedicine–An overview. In: Proceedings of the International Conference on Industrial Engineering and Operations Management; 2022 Aug; Nsukka, Nigeria. p. 5–7. doi:10.4018/979-8-3693-3876-6.ch005
- Musa S, Ramatu AA, Haliru L, Abigail D, Gumbi S. Establishing a paediatric telemedicine centre in a low-resource setting: Experience and challenges from a teaching hospital in Kaduna, Nigeria. Sri Lanka J Child Health. 2023;52(2):155–60. doi:10.4038/sljch.v52i2.10548
- Odilibe IP. Telemedicine and rural healthcare in Africa: A review of accessibility and impact. World J Adv Res Rev. 2024;21(2):421–31. doi:10.30574/wjarr.2024.21.2.0475
- Nwankwo OC, Chukwuma IO, Uche MA. Barriers to telemedicine adoption in Nigeria: A focus on digital infrastructure. J Public Health West Afr. 2023;12(4):98–107.
- Onyeka TC, Nwankwo CH. Geographic and infrastructural barriers to healthcare access in Nigeria’s Niger Delta: A qualitative study of health professionals and community residents. Afr J Prim Health Care Fam Med. 2020;12(1):a2310.
- Amaize N, Oribuyaku GO, Jombo ETA. Healthcare delivery challenges in the riverine communities of the Niger Delta region, Nigeria. Int J Community Med Public Health. 2016;3(11):3170–5.
- Nigeria Magazine. The state of healthcare in Nigeria: challenges and prospects. Nigeria Magazine. 2022 Mar 15 [cited 2025 Sep 2]. Available from: https://nigeriamag.com/the-state-of-healthcare-in-nigeria-challenges-and-prospects
- Omoleke II, Taleat BA. Contemporary issues and challenges of health sector in Nigeria. Int J Dev Strategies Humanit Manage. 2023;13(2):82–90. Available from: https://internationalpolicybrief.org/wp-content/uploads/2023/10/ARTICLE7-40.pdf
- Kruse CS, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J Telemed Telecare. 2018;24(1):4–12. doi:10.1177/1357633X16674087
- Aregbeshola BS, Khan SM. Primary health care in Nigeria: 24 years after Olikoye Ransome-Kuti's leadership. Front Public Health. 2018;6:48. doi:10.3389/fpubh.2017.00048
- Dorsey ER, Topol EJ. State of telehealth. N Engl J Med. 2020;375(2):154–61. doi:10.1056/NEJMra1601705
- Alvandi M. Telemedicine and its role in revolutionising healthcare delivery. Am J Accountable Care. 2020;8(1):17–8.
- Almathami HKY, Win KT, Vlahu-Gjorgievska E. Barriers and facilitators that influence telemedicine-based, real-time, online consultation at patients’ homes: Systematic literature review. J Med Internet Res. 2020;22(2):e16407. doi:10.2196/16407
- Adedini SA, Odimegwu C, Bamiwuye O, Fadeyibi O, De Wet N. Barriers to accessing health care in Nigeria: Implications for child survival. Glob Health Action. 2014;7:23499. doi:10.3402/gha.v7.23499

This work is licensed under a Creative Commons Attribution 4.0 International License.

